The COVID-19 pandemic has delayed access to endoscopy, potentially delaying the diagnosis of Barrett’s esophagus and esophageal cancer. A new study suggests that a noninvasive “sponge on a string” (Cytosponge) plus biomarker panel could help to identify individuals who are at high risk.
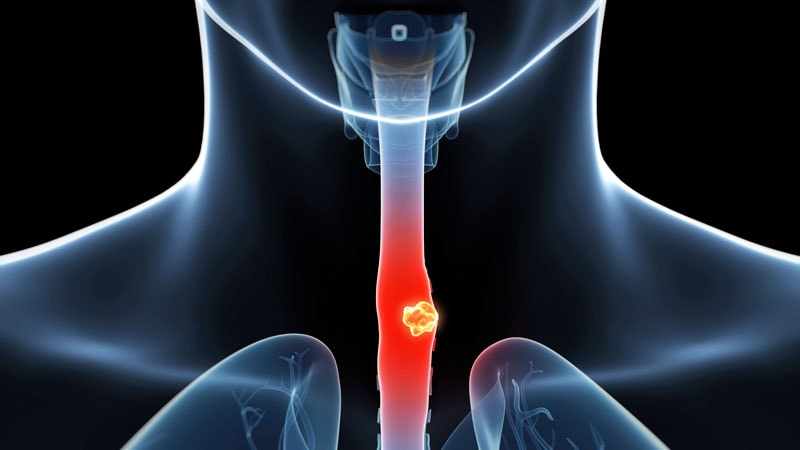
Cytospoinge is an esophageal cell collection device, developed originally at the Medical research Council in the UK and licensed to Covidien (now Medtronic). It is a small capsule-shaped device, about the size of a multivitamin, that is swallowed, but it has a small string attached. Once inside the stomach, the capsule dissolves, and the sponge inside expands. The string is then gently pulled to retract the sponge, but along the way it collects cells from the entire length of the esophagus, the company explains on its website.
Using the Cytosponge before scheduling an endoscopy could proactively test people with regular heartburn — a potential risk factor for Barrett’s esophagus and esophageal cancer, the researchers explain. This has the potential to rule out people who do not need an endoscopy, saving them time and discomfort from an invasive procedure.
“While it won’t completely replace endoscopy, it should reduce unnecessary endoscopy procedures,” commented senior author Rebecca C. Fitzgerald, MD, from the Hutchison/MRC Research Center in Cambridge, United Kingdom, who is named on a patent for the device,.
“On the other hand, it can identify more of the people at risk who often go undiagnosed,” she added. Previous research from Fitzgerald and her colleagues found that the Cytosponge plus a biomarker called TFF3 can detect 10 times more cases of Barrett’s esophagus than an endoscopy procedure.
In the latest study, published online on January 11 in The Lancet, the teamshowed that the Cytosponge and biomarker panel findings could be used, alongside clinical risk factors, to prioritize patients for endoscopy. People who are deemed to be at low risk of progression (no clinical risk factors or Cytosponge findings, which accounts for >50% of these patients) could potentially avoid endoscopy and have Cytosponge follow-up, they conclude.
“Most patients with cancer are diagnosed late and do not know that they had Barrett’s esophagus, so we need easier methods to identify individuals at risk,” Fitzgerald commented to Medscape Medical News,
In an accompanying editorial, Michael Vieth and Markus F. Neurath, from the Friedrich-Alexander University Erlangen-Nuremberg in Germany, support the quest for finding easier screening options for Barrett’s esophagus.
“Cytosponge in Barrett’s oesophagus has several technical advantages: it is easy to apply, larger areas of oesophageal surface tissue can be assessed compared with a set of biopsies, it is a standardised procedure, and it is compatible with subsequent techniques, such as immunohistochemistry,” they write.
“However, Cytosponge also has some potential disadvantages, such as the high cost for a single-use device,” they point out, adding that “it remains to be seen whether it will be feasible to use Cytosponge in all countries in real-world conditions.”
“Endoscopy is still the key technology for patients with relevant cancer risk,” they write.
While invasive, endoscopy is cost-effective.
Dr Anton Bilchik
“While invasive, endoscopy is cost-effective,” noted an expert approached for comment, Anton Bilchik, MD, PhD, from Saint John’s Cancer Institute in California. “We don’t really know the cost for a Cytosponge evaluation,” he added. Also, “if patients have a positive Cytosponge bimarker test, then they’ll need a biopsy, so they’ll still have an endoscopy and potentially end up paying for two procedures,” he said in an interview with Medscape Medical News.
The Cytosponge biomarker test is revolutionary to the field, Bilchik commented, but more work needs to be done. These findings need to be reproduced in other centers, and there is a need to see if other pathologists not affiliated with the research can produce similar results, he commented.
The Cytosponge is currently being used in large pilot studies conducted by the National Health Service (NHS) England and the NHS Scotland, Fitzgerald told Medscape Medical News. Since August 2020, the Cytosponge has been used in over 5000 clinical procedures, she added.
Fitzgerald said her team is also working to expand the Cytosponge to detect another type of esophageal cancer, known as squamous cell carcinoma.
Medtronic, the company that develops the Cytosponge, told Medscape Medical News that it is planning a full US commercial launch with promotional support expected in the next 18 months.
Lancet Oncol. Published online January 11, 2022. Full text, Editorial
For more news, follow Medscape on Facebook, Twitter, Instagram, and YouTube.