Hypertrophic cardiomyopathy (HCM) is the most common form of hereditary heart disease, affecting 1 in 200-500 people. Of all the heterogenous manifestations associated with HCM, including left ventricular outflow tract obstruction and heart failure, sudden cardiac death (SCD) is the most devastating. SCD occurs in approximately 0.5% of patients per year, most commonly from ventricular tachyarrhythmias; pulseless electric activity and asystole are other possible causes. Multimodality imaging is critical not only to the diagnosis of HCM but also in the prognostic evaluation. Moreover, SCD risk stratification is essential to managing patients with HCM. Here, we review current recommendations and recent studies evaluating additional prognostic markers in HCM to enhance SCD risk stratification.
Starting Point: Initial Evaluation
A thorough history and physical examination are fundamental to the evaluation of HCM and to determine a patient’s risk factors for SCD. The strongest risk factors for SCD are a history of prior resuscitated cardiac arrest, ventricular fibrillation, and/or sustained ventricular tachycardia. The 2020 American Heart Association/American College of Cardiology (AHA/ACC) and the 2014 European Society of Cardiology (ESC) guidelines recommend conventional 12-lead electrocardiography and 48-hour ambulatory electrocardiographic monitoring for the initial evaluation of HCM. In addition, both guidelines note that a longer-term surface or implantable monitoring device may be considered if there is ongoing clinical concern. It’s important to determine whether a patient has a family history of SCD, particularly if more than one first-degree relative and possibly other close relatives aged ≤ 50 years are affected. Approximately 15%-25% of patients with HCM have unexplained syncope, the onset of which may occur within 6 months of initial evaluation; younger patients (aged < 18 years) have a worse prognosis. Nonsustained ventricular tachycardia also confers worse prognosis, especially in patients aged < 30 years. Abnormal blood pressure response to exercise can occur in up about 25% of patients with HCM as a consequence of suboptimal diastolic filling and/or left ventricular outflow tract obstruction. Although SCD is more common in adolescent and young adult patients (aged < 35 years), it occurs in all age groups, making the relationship between SCD and age more complex.
Multimodality Imaging
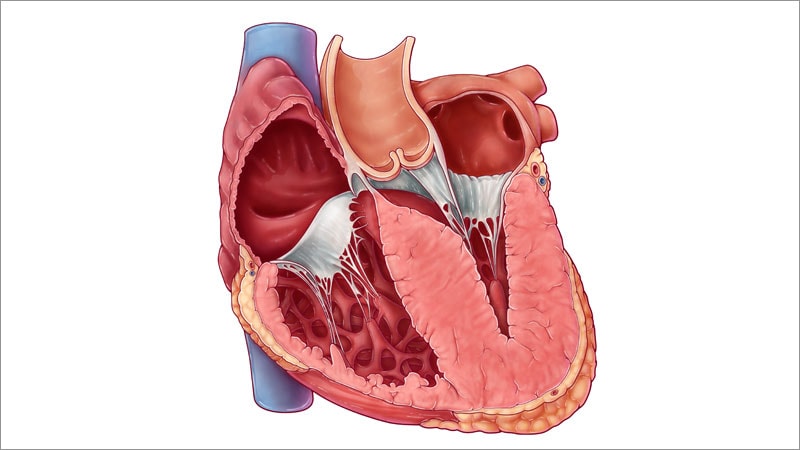
Echocardiography is the first-line imaging modality for HCM, and cardiac MRI is the gold standard for chamber quantification and tissue characterization. Both are essential for SCD risk stratification in patients with HCM. Key parameters include the following:
-
Maximal left ventricular wall thickness. Echocardiographic or cardiac MRI studies showing maximal left ventricular wall thickness (≥ 30 mm) positively correlate with SCD risk.
-
Left ventricular systolic impairment. Although a left ventricular ejection fraction < 50% (late-stage HCM) is rare (occurring in in only 3.5% of patients), its presence often leads clinicians to recommend defibrillator implantation (10% per year).
-
Left atrial dimensions. These measurements are controversial as risk factors for SCD. Although early studies showed left atrial diameter as a continuous parameter to confer SCD risk, left atrial volume index, which more accurately reflects size, is less studied but similarly shows associations with adverse outcomes.
-
Left ventricular outflow tract obstruction (LVOT) ≥ 30 mm Hg. In addition to its prevalence in two thirds of HCM patients at rest and with provocation (eg, Valsalva maneuver, amyl nitrate inhalation, exercise), LVOT obstruction is also associated with SCD.
-
Apical aneurysm. In a minority of patients with HCM, the presence of an apical aneurysm often involves extensive fibrosis — approximately 2% of patients with HCM overall. Apical aneurysm, which is best assessed with contrast echocardiography or MRI, is another important predictor of SCD.
-
Late gadolinium enhancement on MRI. The presence of late gadolinium enhancement suggests myocardial fibrosis and is seen in approximately 50% of patients with HCM. In several studies and meta-analyses, late gadolinium enhancement conferred a twofold to threefold risk for SCD.
Novel Parameters in Risk Stratification
Contemporary studies have identified prognostic markers in HCM that are not currently part of existing risk models. In a systematic review of 15 observational studies and 3154 patients with HCM, abnormal left ventricular global longitudinal strain on echocardiography was associated with ventricular arrhythmias and cardiovascular events. However, heterogeneity in strain software, thresholds, and outcomes prevent determination of a precise recommendation for the optimal strain cutpoint value. Recent cardiac MRI studies in patients with HCM found that elevated T1 extracellular volume and T2 signals and values are associated with cardiovascular events (including cardiac death) and have prognostic value in predicting SCD risk. In addition, surgical myectomy may downmodulate SCD risk, so risk scores may not perform appropriately. Further studies are needed to assess how novel markers interact with traditional risk factors before they may be incorporated into HCM risk stratification models.
Current Risk Models
The two main models for SCD risk in HCM are the one published in the AHA/ACC Guideline for the Diagnosis and Treatment of Patients With Hypertrophic Cardiomyopathy, and the HCM Risk-SCD model in the ESC Guidelines on Diagnosis and Management of Hypertrophic Cardiomyopathy. The AHA/ACC guidelines initially listed risk factors, including SCD in first-degree family members, unexplained syncope, nonsustained ventricular tachycardia, maximal left ventricular wall thickness ≥ 30 mm, and abnormal blood pressure response to exercise (the latter was removed after update). On the basis of findings from studies, including an observational study of 2094 patients with HCM, the guidelines were subsequently updated to include additional risk modifiers, such as apical aneurysm and late gadolinium enhancement on MRI.
In contrast to the AHA/ACC model, the ESC model directly estimates the 5-year risk for SCD to guide management decisions in patients with HCM, using clinical parameters of left ventricular maximal wall thickness, left atrial diameter, maximal LVOT gradient (at rest and with the Valsalva maneuver), family history of sudden cardiac death, nonsustained ventricular tachycardia, and age. Calculated risks are categorized as low (< 4%), intermediate (4%-6%), or high (> 6%) and recommendations regarding implantable cardioverter-defibrillator (ICD) therapy are provided (ie, “not indicated,” “may be considered,” and “should be considered”).
Clinicians should be aware of limitations associated with each of these risk models. The ESC model, which was externally assessed in EVIDENCE-HCM, an international cohort study of 3703 patients with HCM, demonstrated moderate discriminative ability (c-statistic, 0.70) to support its use in ICD selection. The previously mentioned observational study of 2094 patients with HCM who had ICD intervention sought to assess the specificity and sensitivity of the AHA/ACC and ESC models. It found that the enhanced AHA/ACC guidelines, ESC model (combined high-risk and intermediate-risk scores ≥ 4% over 5 years) and ESC model (high-risk score ≥ 6% over 5 years) had sensitivities of 95%, 58%, and 34%, respectively; specificities of 78%, 81% and 92%, respectively; and c-statistics of 0.81 and 0.74 (ESC models combined), respectively, to discriminate SCD events. These findings suggest the enhanced AHA/ACC guidelines, which include apical aneurysm and late gadolinium enhancement ≥ 15%, are a more effective prediction model for SCD in HCM than the ESC model. Another recent study of 1809 patients with HCM also found that the ESC model did not perform well, although myectomy may have reduced the risk for SCD.
Furthermore, the AHA/ACC and ESC criteria do not appear to perform well in athletes with HCM. For example, in a small cohort study of 35 athletes, a high percentage of athletes was considered low-risk for SCD according to both models (89% per the ESC model and 77% per the AHA/ACC guidelines). There was no indication for prophylactic ICD in any of the participants. All of the participants in the study were advised to discontinue their exercise program; however, 15 participants continued with regular exercise. Over a follow-up period of 9 years, the authors found no differences in occurrence of symptoms between the athletes who continued with an exercise program and those who were sedentary. Regardless of exercise status, 20% of participants experienced HCM-related symptoms, which suggests that low-risk patients may develop symptoms regardless of their activity level. Additional, larger studies are needed to further investigate these findings. In the meantime, we recommend using the ACC/AHA updated guidelines algorithm as a starting tool and incorporating newer imaging modifiers to optimize the accuracy of SCD risk stratification.
Management and the ICD
One of the goals of SCD risk stratification is to determine which patients would benefit from an ICD — a cornerstone of HCM management. ICD therapies include both shock delivery and anti-tachycardia pacing to help terminate ventricular tachycardia and avoid the need for shock. Survival of prior SCD, ventricular fibrillation, and sustained ventricular tachycardia, with a life expectancy > 1 year are class I indications for ICD as a secondary prevention in the AHA/ACC guidelines (Table). The AHA/ACC guidelines base class II indications on the presence of traditional and enhanced risk factors, whereas the ESC guidelines use the estimated 5-year SCD risk based on their model. ICDs are not routinely recommended for every patient, especially those at low risk.
Other items to review before and after ICD implantation include counseling patients about complications (eg, inappropriate shocks, lifestyle restrictions, occupational and other activities). In selected patients without pacing indications, the subcutaneous ICD has become an alternative to transvenous systems. Risk evaluation should be assessed at baseline and every 1-2 years, and when there is a change in clinical status.
Table. Indications for Implantable Cardioverter-Defibrillator in HCM (Modified)
| 2020 ACC/AHA Guidelines | 2014 ESC Guidelines |
|---|---|
| Class I Indication
Class IIa Indications
Class IIb Indications
Class III Contraindication
|
Class I Indications
Class IIa Indication
Class IIb Indication
Class III Contraindication
|
In conclusion, sudden cardiac death is an infrequent but devastating complication of HCM, making risk assessment and stratification critical in its management. Clinical parameters, multimodality imaging, markers, and risk models have important roles in the evaluation of SCD risk to guide HCM management. We advocate utilizing the updated AHA/ACC prediction model along with novel imaging biomarkers, as discussed, for SCD risk stratification and ICD selection. Accurate risk evaluation is essential to improving clinical outcomes and SCD prevention in these patients.
Follow theheart.org | Medscape Cardiology on Twitter
Follow Medscape on Facebook, Twitter, Instagram, and YouTube