Practice Essentials
Infertility in men can result from deficiencies in sperm formation, concentration, or transportation. This general division allows an appropriate workup of potential underlying causes of infertility and helps define a course of action for treatment.
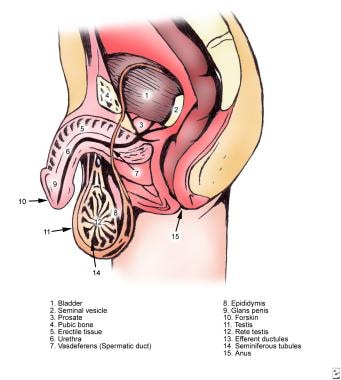
The image below depicts male ductal anatomy.
Male infertility. Normal male ductal anatomy.
Signs and symptoms
The initial step in the evaluation of an infertile male is to obtain a thorough medical and urologic history. Such a history should include consideration of the following:
Duration of infertility
Previous fertility in the patient and the partner
Timing of puberty (early, normal, or delayed)
Childhood urologic disorders or surgical procedures
Current or recent acute or chronic medical illnesses
Sexual history
Testicular cancer and its treatment
Social history (eg, smoking and alcohol use)
Medications
Family history
Respiratory disease
Environmental or occupational exposure
Spinal cord injury
The physical examination should include a thorough inspection of the following:
Testicles (for bilateral presence, size, consistency, symmetry)
Epididymis (for presence bilaterally, as well as any induration, cystic changes, enlargement, tenderness)
Vas deferens (for presence bilaterally, defects, segmental dysplasia, induration, nodularity, swelling)
Spermatic cord (for varicocele)
Penis (for anatomic abnormalities, strictures, or plaques)
Rectum (for abnormalities of the prostate or seminal vesicles)
Body habitus
Depending on the findings from the history, detailed examination of other body functions may also be warranted.
See Presentation for more detail.
Diagnosis
The semen analysis is the cornerstone of the male infertility workup and includes assessment of the following:
Semen volume (normal, 1.5-5 mL)
Semen quality
Sperm density (normal, >15 million sperm/mL)
Total sperm motility (normal, >40% of sperm having normal movement)
Sperm morphology (sample lower limit for percentage of normal sperm is 4%)
Signs of infection – An increased number of white blood cells (WBCs) in the semen may be observed in patients with infectious or inflammatory processes
Other variables (eg, levels of zinc, citric acid, acid phosphatase, or alpha-glucosidase)
Other laboratory tests that may be helpful include the following:
Antisperm antibody test
Hormonal analysis (FSH, LH, TSH, testosterone, prolactin)
Genetic testing (karyotype, CFTR, AZF deletions if severe oligospermia (< 5 million sperm/mL)
Imaging studies employed in this setting may include the following:
Transrectal ultrasonography
Scrotal ultrasonography
Vasography
An abnormal postcoital test result is observed in 10% of infertile couples. Indications for performing a postcoital test include semen hyperviscosity, increased or decreased semen volume with good sperm density, or unexplained infertility.
If the test result is normal, consider sperm function tests, such as the following:
Capacitation assay
Acrosome reaction assay
Sperm penetration assay
Hypoosmotic swelling test
Inhibin B level
Vitality stains
Testicular biopsy is indicated in azoospermic men with a normal-sized testis and normal findings on hormonal studies to evaluate for ductal obstruction, to further evaluate idiopathic infertility, and to retrieve sperm.
See Workup for more detail.
Management
The following causes of infertility, if identified, can often be treated by medical means:
Endocrinopathies
Antisperm antibodies
Retrograde ejaculation
Poor semen quality or number
Lifestyle issues
Infections
Surgical interventions to be considered include the following:
Varicocelectomy
Vasovasostomy or vasoepididymostomy
Transurethral resection of the ejaculatory ducts
Sperm retrieval techniques
Electroejaculation
Artificial insemination
Assisted reproduction techniques
In vitro fertilization
Gamete intrafallopian transfer (GIFT) and zygote intrafallopian transfer (ZIFT)
Intracytoplasmic sperm injection
See Treatment and Medication for more detail.