Practice Essentials
A successful kidney transplant offers enhanced quality and duration of life and is more effective (medically and economically) than long-term dialysis therapy for patients with chronic or end-stage kidney disease.
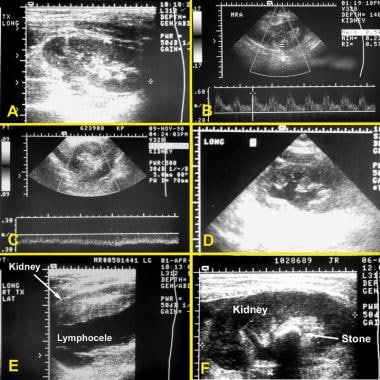
Transplantation is the renal replacement modality of choice for patients with diabetic nephropathy and pediatric patients. The ultrasonograms below illustrate several scenarios associated with kidney transplantation.
Kidney transplantation ultrasonograms. (A) Normal kidney. (B) Color Doppler ultrasonogram documenting normal perfusion to the kidney. (C) Color Doppler ultrasonogram showing absence of perfusion in a patient with thrombosis. (D) Hydronephrosis. (E) Lymphocele. (F) Stone in a kidney transplant.
Pretransplantation evaluation
Candidates for kidney transplantation undergo an extensive evaluation to identify factors that may have an adverse effect on outcome. Virtually all transplant programs have a formal committee that meets regularly to discuss the results of evaluation and select medically suitable candidates to place on the waiting list.
Emphasize identifying and treating all coexisting medical problems that may increase the morbidity and mortality rates of the surgical procedure and adversely impact the posttransplant course. In addition to a thorough medical evaluation, evaluate the social issues of the patient to determine conditions that may jeopardize the outcome of transplantation, such as financial and travel restraints or a pattern of noncompliance.
Laboratory studies in transplant candidates
Blood chemistries
Liver function tests
Complete blood count (CBC)
Coagulation profile
An infectious profile should include the following:
Hepatitis B and C serologies
Epstein-Barr virus (EBV) serologies (IgM and IgG)
Cytomegalovirus (CMV) serologies (IgM and IgG)
Varicella-zoster virus (VZV) serologies (IgM and IgG)
Rapid plasma reagin (RPR) test for syphilis
HIV
Purified protein derivative (PPD) – Tuberculosis skin test with anergy panel, when indicated
Urinalysis, urine culture, and cytospin should be ordered when indicated.
Diagnostic procedures
A complete cardiac workup, including angiography, is not necessary in every transplant candidate, but patients with a significant history, symptoms, type 1 diabetes, or hypertensive renal disease should undergo a thorough evaluation to rule out significant coronary artery disease (CAD). The following procedures are indicated:
12-lead ECG
Chest radiography (posteroanterior [PA] and lateral views)
Exercise and dipyridamole thallium scintigraphy
2-dimensional echocardiography with Doppler (with or without dobutamine)
Coronary arteriography (if indicated)
Special procedures may be indicated in selected patients on the basis of findings revealed in the history and physical examination.
Studies in transplant recipients
Transplant ultrasonography to identify urinary obstruction, as well as fluid collections suggesting urine extravasation, abscess, pyelonephritis, or wound infection
Color flow Doppler ultrasonography to evaluate vascular occlusion or stenosis
Renal biopsy usually required for definitive diagnosis of most renal graft dysfunction
Lumbar puncture in cases of suspected meningitis, particularly that believed to be caused by
Listeria species
Immunologic evaluation
Recipients of kidney transplants undergo an extensive immunologic evaluation that primarily serves to avoid transplants that are at risk for antibody-mediated hyperacute rejection. The immunologic evaluation consists of the following 4 components:
ABO blood group determination
Human leukocyte antigen (HLA) typing
Serum screening for antibody to HLA phenotypes
Crossmatching
Kidney transplant candidates with preformed, donor-specific antibodies may undergo a pretransplant desensitizing protocol. If successful, this protocol reduces antibody levels to the point where kidney transplantation becomes feasible.
Pretransplant surgical interventions
The medical workup may reveal circumstances that necessitate surgical intervention to prepare the patient for kidney transplantation. Such interventions may include the following:
Native kidney nephrectomy or nephroureterectomy – Reserved for specific indications, such as large polycystic kidneys, significant proteinuria, or chronic reflux disease
Cholecystectomy – For patients with gallstones
Splenectomy – May be indicated for ABO-incompatible kidney transplantations
Management
In addition to the surgical transplantation procedure itself, management includes the following:
Organ procurement
Provision of immunosuppressive therapy to the recipient
Short- and long-term follow-up to look for indications of renal allograft dysfunction and other complications
Organ procurement
Identification of potential donors
Assessment of donor suitability
Determination of donor brain death
Medical management of donor
Immunosuppressive therapy
All kidney transplant recipients require life-long immunosuppression to prevent a T-cell alloimmune rejection response. The goals are as follows:
Prevent acute and chronic rejection
Minimize drug toxicity and rates of infection and malignancy
Achieve the highest possible rates of patient and graft survival
Immunosuppressive agents may be divided into 2 broad categories, as follows:
Antirejection induction agents (polyclonal antisera, mouse monoclonals, humanized monoclonals)
Maintenance immunotherapy agents (prednisone, azathioprine, mycophenolate mofetil, cyclosporine, tacrolimus, sirolimus, belatacept)
Complications
The critical considerations in medical followup are as follows:
Rejection
Nephrotoxicity of calcineurin inhibitors (ie, cyclosporine, tacrolimus)
Recurrence of native kidney disease
Anatomic complications of surgery are as follows:
Renal artery thrombosis
Renal artery stenosis
Urine leaks from disruption of the anastomosis
Ureteral stenosis and obstruction (relatively late complications)
Lymphocele
Allograft dysfunction and rejection may occur as follows:
Hyperacute rejection of the renal allograft occurs within hours of the transplant; nephrectomy is indicated
Acute rejection appears within the first 6 months after transplantation (15% of cases)
Chronic rejection occurs more than 1 year after transplantation and is a major cause of allograft loss
Other complications include the following:
Infection
Malignancy
Liver disease
Hypertension
Cardiovascular disease