Practice Essentials
Acute acalculous cholecystitis (AAC) represents inflammation of the gallbladder in the absence of demonstrated calculi (see the image below). The disease process of AAC is distinct from that of the calculous variety, in which the primary initiating event is believed to be obstruction of the cystic duct. Acalculous cholecystitis typically occurs as a secondary event in patients who are hospitalized and are acutely ill with another disease.
Compared to acute calculous cholecystitis, AAC is associated with more complications and a worse prognosis. AAC is more often associated with gallbladder gangrene, perforation, and empyema.
AAC constitutes approximately 10% of all cases of acute cholecystitis and occurs in 0.2-0.4% of critically ill patients.
The diagnosis often is difficult and is often delayed because of comorbidities that decrease sensitivity and specificity of clinical and imaging evaluation. A high degree of suspicion is required on the part of the physician. A much higher rate of complications is observed in patients with acalculous cholecystitis (eg, gangrene, perforation) because of the more fulminant course and coexistent disease. As a result, some authors propose the term necrotizing cholecystitis to reflect the fact that acalculous cholecystitis does not simply represent cholecystitis without stones.
Although most acute inflammatory diseases of the gallbladder in adults involve calculous cholecystitis, acute acalculous cholecystitis accounts for 30-50% of acute inflammatory gallbladder disease in pediatric patients.
Preferred examination
Early imaging evaluation is required for patients with acalculous cholecystitis, and frequently, multiple diagnostic tests are performed. No single imaging study is ideal.
The 3 primary imaging modalities often are complementary, with ultrasonography (US) or computed tomography (CT) scanning providing anatomic information and evaluation of adjacent structures and cholescintigraphy providing functional information.
US and cholescintigraphy should be the initial imaging tests performed to evaluate possible AAC. Ultrasound is often the preferred modality because of its availability, lack of radiation, and high specificity for the biliary system.
A CT scan should be done if US is inconclusive, and CT scanning is preferred if other diseases in the differential diagnosis are more likely or if CT scanning needs to be performed for another indication.
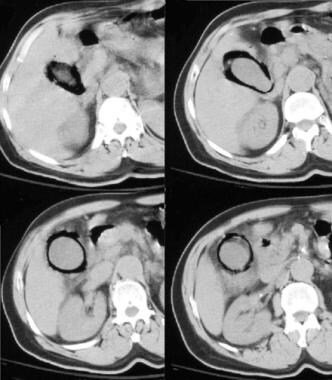
Emphysematous cholecystitis, which can occur as a complication of acute cholecystitis, is seen in the images below.
Abdominal radiograph of acalculous emphysematous cholecystitis demonstrating curvilinear air pattern conforming to the shape of the gallbladder wall.
CT images of emphysematous cholecystitis.
Limitations of techniques
All available modalities have a significant false-positive and false-negative rate and generally are better at excluding, rather than confirming, the presence of acalculous cholecystitis.
Although it is unusual for acalculous cholecystitis to occur in patients with a normal gallbladder, on US and cholescintigraphy examinations, the gallbladder may be found to be normal early in the course of the disease. For patients who continue to experience clinical deterioration and for whom clinical evaluation is not possible or fails to demonstrate an alternative source, many authors recommend maintaining a low threshold for instituting empiric, minimally invasive therapy in the form of percutaneous cholecystostomy.