Overview
Coronary artery disease (CAD) is a complex disease that causes reduced or absent blood flow in one or more of the arteries that encircle and supply the heart. The disease may be focal or diffuse. Apart from rare congenital anomalies (birth defects), coronary artery disease is usually a degenerative disease, uncommon as a clinical problem before the age of 30 years and common by the age of 60 years. One in four people will have a heart attack. The first recognized symptom may be death. The term coronary is derived from crown, referring to the way these arteries sit on the heart.
The American College of Radiology notes that coronary artery disease has a long asymptomatic latent period and that early targeted preventive measures can reduce mortality and morbidity. Imaging modalities for evaluating patients at increased risk for CAD include radiography, fluoroscopy, multidetector CT, ultrasound, MRI, cardiac perfusion scintigraphy, echocardiography, and positron emission tomography (PET).
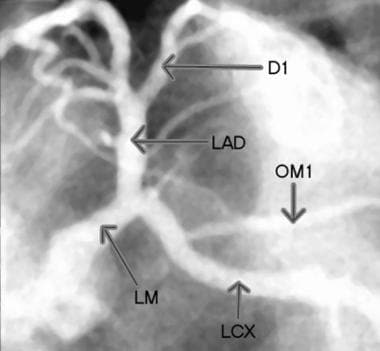
See the images below depicting the coronary arteries and CAD.
Selective injection image of the left coronary arteries. D1 = first diagonal, LAD = left anterior descending artery, LCX = left circumflex, LM = left main coronary artery, and OM1= first obtuse marginal.
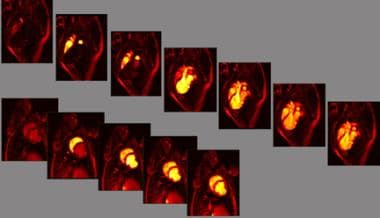
Contrast-labeled blood to the heart is used to identify the territory at risk. The results of this assessment of the delayed arrival compares favorably to the findings of radionuclide stress imaging, and stress induction of ischemia is not required to identify the zone at risk.
Compared with radionuclide images of blood delivery, MRIs and CT scans improve resolution, depiction of the functional effect and the relationship to the coronary supply, and identification of the area at risk without stress. The advantage of radionuclide imaging is primarily its predictive value; stress echocardiography has similar predictive value. MRI and CT have been less available than other studies; therefore, data on their value are relatively limited.
Stable and unstable lesions
Lesions that cause blockages in the coronary arteries may be stable or unstable. Unstable lesions activate blood clotting and/or vascular spasm. Indications that CAD may be unstable include recent onset or familiar symptoms that are increasing in frequency, in duration, or in severity or with decreasing exertion tolerance or at rest. The term “chest pain” is a code phrase — the symptoms of CAD do not have to be in the chest and do not have to include pain. I prefer the phrase “heart warning” symptoms. When a warning light is activated, you should resolve the problem quickly even if it is low in intensity.
Unstable symptoms of CAD may represent a threatened heart attack. After as little as 5 minutes, a wall of the heart may stop functioning but still be salvageable — that is called stun. After as little as 10-20 minutes permanent damage may accumulate, summarized by the phrase “time is muscle.” If the symptoms are new or if they are familiar but unstable or are not reliably fully resolved in 5 minutes, emergency help is recommended because “time is muscle.” Intervention completed within 60 minutes improves outcome. The symptoms of a threatened heart attack may be very mild.
Ischemia
When the heart has inadequate blood supply (ie, ischemia), pressure may be felt in the chest that moves to the left arm; one may feel weak, sweaty, or short of breath or nauseated; palpitations (ie, change in heart rhythm) may occur; or there may be a sensation of pressure or tightness just in the chest, neck, or arms.
Many patients mistake the heart warning symptoms for heartburn or gas. If symptoms occur that may represent inadequate blood supply to the heart, one should rest immediately and take nitroglycerin, if available. If symptoms last more than 5 minutes, occur at rest, or keep coming back, one should call 911, chew a full-sized aspirin (325 mg) if not allergic, and continue taking nitroglycerin every 5 minutes as long as it does not cause dizziness or light-headedness.
For excellent patient education resources, see eMedicineHealth’s Cholesterol Center. Also, visit eMedicineHealth’s patient education articles Chest Pain, Coronary Heart Disease, and Heart Attack.
Severity of CAD
The severity of CAD is defined several ways, including the following:
Anatomically, by visualizing the blood vessel branches and any blockages to blood flow along the pathways
Functionally, by estimating blood delivery to tissue supplied by each branch vessel
Clinically, by determining what symptoms correspond to inadequate blood delivery, what level of activity causes them, what relieves them, and the pattern of occurrences
Such patterns are described as unstable if the pattern includes variable or accelerating frequency, variable or increasing severity or changing character of symptoms, or variable or decreasing exercise threshold or if symptoms continue or recur just after a heart attack.
In addition, one examines the consequences, including the location and extent of reversible and of permanent impairment, motion and thickening of affected segments of the heart, and whether the damage is causing or sustaining life-threatening arrhythmias.
One also evaluates the patient’s overall cardiac performance, which is typically expressed as the ejection fraction (EF), or percentage of the contents the left ventricle pumps forward in a heartbeat, and exertion tolerance, graded 1-4 (1=normal, 4=bedridden).
The TIMI (Thrombolysis in Myocardial Infarction) risk score looks at 7 factors that point to bad outcomes:
Age 65 years or older
At least 3 risk factors for coronary artery disease
Prior coronary stenosis of 50% or more
ST-segment deviation on electrocardiogram at presentation greater than 0.5 mm
At least 2 anginal events in prior 24 hours
Use of aspirin in prior 7 days
Elevated serum cardiac markers
TIMI risk scores have the following risk of all-cause mortality, new or recurrent MI, or severe recurrent ischemia requiring urgent revascularization within the first 2 weeks: 1=5%, 2=8%, 3=13%, 4=20%, 5=26%, 6/7=41%.
Imaging of CAD
At present, achieving the best resolution on images of the coronary arteries requires catheterization, injection of an iodinated contrast agent, and use of a radiographic technique. As an alternative, multidetector-row CT (MDCT) or MRI may be used to clarify coronary anatomy and to determine whether a vessel is occluded.
Stress imaging has a complementary role in depicting zones with inducible ischemia (blood supply inadequate for the demands of the tissue). Stress may be produced with exercise, an infusion of a medication that increases the strength of cardiac contractions (eg, dobutamine), or an infusion of a medication (eg, adenosine, dipyridamole) that dilates the vessels and thereby reduces the delivery of blood to diseased branches.
More than a decade ago, MRI was shown to be capable of imaging the coronary arteries and demonstrating stenoses without catheterization or injection of contrast material.
MDCT is now proving to be a fast and useful alternative for defining the coronary anatomy.
MRI takes more time than MDCT and generally provides less detail of the coronary anatomy, but it avoids ionizing radiation and the use of iodinated contrast agent.
Advances in MRI and CT have markedly improved the speed and resolution of imaging, making these modalities useful in the clinical evaluation of CAD while improving their safety and convenience. In addition to defining the anatomy, both MRI and CT can be used to identify zones of impaired blood supply by timing of the arrival of contrast agent–labeled blood.
In addition, MRI is useful in identifying the location and thickness of myocardial scars. Although neither MRI nor CT has replaced coronary angiography (XRA) as the clinical standard for the diagnosis of coronary stenosis, their use in determining if a vessel is open is increasing. Recently, 64-slice multidetector-row CT angiography (CTA) has shown potential as an alternative to coronary angiography for the identification of coronary blockages.
In a study of 15,207 intermediate likelihood patients without known CAD, the severity of CAD on coronary CTA was predictive of the need for invasive coronary artery catheterization or revascularization. This suggests that coronary CTA may be an effective gatekeeper for invasive catheterization.
Assessment of tissue viability
The amount of impairment or damage caused by stenosis obstructing a coronary artery depends on how much of the myocardium the vessel supplies, the severity of the stenosis and any superimposed spasm, the level of demand in the tissue it supplies, and the condition of the tissue it supplies.
When demand exceeds supply, the tissue becomes ischemic, which means blood supply is insufficient to maintain normal metabolism. Myocardial ischemia may cause chest pain, fatigue, shortness of breath, or another form of reduced exertion tolerance.
Ischemia may have no symptoms but may be detected as impaired blood delivery, impaired contractile function (wall motion or wall-thickening abnormality on dynamic cardiac imaging series), or interference with the movement of ions (resulting in depolarization and repolarization abnormalities on ECGs as ST-segment shifts, changes in ST and T waves, and/or rhythm abnormalities); and/or it may be detected when a blood test shows a release of enzymes (creatine kinase-MB [CK-MB], troponin-I, troponin-T) from the heart muscle.
Ischemia may deplete high-energy phosphate carriers (eg, creatine, adenosine) that are needed for muscle contraction. Depletion may occur to the point that impaired motion may persist even when ischemia is relieved. Transiently impaired contractile function of muscle that persists after the relief from ischemia is called stun, and long-term dysfunction of viable muscle is called hibernation.
Dead tissue converted to scar likewise loses contractile function. Therefore, a key issue when a region of heart wall shows loss of function is the determination of whether the myocardium is still viable. Persistent wall-motion abnormality at rest shown by imaging (echocardiography, MRI, CT, coronary angiography) can raise the issue of tissue viability and, in particular, whether repairing a blockage in the blood supply is likely to be beneficial.
If a region is thin and akinetic (no motion), it is more likely to scar (dead myocardium) than if it is not. However, when in doubt, viability tests are appropriate. For example, viability can be identified by performing phosphorus-31 MRI and by reporting for each region the relative concentrations of creatine phosphate; inorganic phosphate; and adenosine monophosphate, diphosphate, and triphosphate.
Although MRI of phosphorylated metabolites and positron emission tomography (PET) of metabolic activity (to assess glucose utilization) can be used to assess tissue viability, an alternative method of equal, if not better, clinical value is imaging by MRI with contrast to identify contrast retention by damaged myocardium. We first observed that phenomenon over a decade ago when studying an animal model of ischemia and infarction while looking at angiogenesis (treatments to promote development of the blood supply).
Another way to identify viability is to examine wall motion at rest and with light stress. Dobutamine stress imaging may be performed with MRI or echocardiography. Dobutamine stress tests are used to detect viability by demonstrating dose-related increases in contractility if the tissue is viable. An increase in the dose of dobutamine may subsequently elicit a decline in contractility associated with induced ischemia—that is, a biphasic response, indicating viable but threatened myocardium.
Early in the development of perfusion imaging
, we observed retention of gadolinium contrast by injured myocardium. Normally, a bolus of contrast agent washes out of the heart walls within 5-10 minutes. Any contrast agent seen in the heart after the agent has washed out of normal zones demarcates injured myocardium.
This technique has since been called MRI scar mapping or delayed enhancement imaging. The fraction of wall thickness that retains gadolinium-based contrast agent 10-20 minutes after a bolus infusion of 20 mL/75 kg indicates viability. The result is an excellent predictor of potential for functional recovery. If the scar is less than one third the thickness of the wall, improvement with revascularization is likely. However, if the scar is more than two thirds the thickness of the wall, improvement after revascularization is unlikely.
MRI scar maps depict contrast retention due to cell disruption. Although acute injury results in slightly enlarged zones of retained contrast agent on MRI, after a week, the defined zone appears the same months to years later and it corresponds on pathology to dead tissue.
Unfortunately, in patients with poor renal function, gadolinium contrast may stay in the body long enough to cause a potentially disabling inflammatory reaction called nephrogenic systemic sclerosis, also known as nephrogenic fibrosing dermopathy (NSF/NFD).
NSF/NFD has been linked to all the gadolinium-based contrast agents. For more information, see Nephrogenic Fibrosing Dermopathy. The disease has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or MRA scans.
Appropriate and timely treatment
When symptoms suggestive of a possible threatened heart attack are present (persisting chest pain or pressure radiating to 1 or both arms or jaw; or unexplained shortness of breath, weakness, sudden sweating, or a serious arrhythmia), an electrocardiogram should be obtained promptly, with continual monitoring for arrhythmia or ischemia (impaired blood supply).
Ambulances have both ECG and rhythm and oxygenation monitoring equipment, as do emergency departments. The ECG can show ST segment shifts and/or T-wave inversions as signs of heart ischemia or injury. However, there are electrically silent areas in the standard monitors. A 12-lead ECG does not detect all of the electrical warning signs of heart damage; more extensive thoracic coverage is desirable.
Preferred examination
If a patient has symptoms, suggestive ECG findings, or imaging results that indicate a need for intervention, coronary angiography by means of catheterization is currently the preferred examination for identifying the culprit lesions and, often, for providing an interventional remedy during a single session.
The patient’s clinical history (age, symptoms, risk factors) provides an estimate of disease likelihood. The basic screening test is stress ECG, which can adjust prognosis depending on the pretest likelihood of disease.
Generally, if the patient has no symptoms and the resting and stress ECGs are normal, the risk of mortality in the next year is low. However, the predictive accuracy of ECG even at peak stress as part of stress testing overall is not good, with as much as one half of all cases of disease missed by ECG. The simple addition of stress testing of B-type natriuretic peptide (BNP) levels in the blood markedly improves the predictive accuracy.
Other ways to improve accuracy are nuclear imaging, echocardiography, MRI, or CT.
Stress nuclear imaging is widely used to assess the patient’s exercise tolerance and to identify zones of inducible ischemia (jeopardized myocardium), which is useful information, even after coronary angiography is performed. PET offers similar rest-stress data and is superior for identifying viable myocardium. Jeopardy and viability are important issues, because if the myocardium is not at risk or if it is not viable, revascularization (bypass or angioplasty) will not help that part of the heart.
Echocardiography to identify wall motion abnormalities has a similar predictive accuracy in patients with intermediate suspicion of CAD, estimated at 80-90%. Echocardiography avoids radiation exposure, which may cause as much as 1 new cancer for every thousand patients studied, but radionuclide imaging (thallium, sestamibi) is preferred if the patient already has old wall motion abnormalities or has poor echo windows (lung blocks the views).
Exercise stress echo may be performed before and after treadmill exercise or during exercise on a supine bicycle. The latter requires more cooperation but allows imaging at every stage, so it may avoid false negatives from rapid recovery or from involvement of all areas (balanced ischemia).
MRI and CT have markedly improved the ability to depict zones of impaired blood supply and to display the coronary anatomy. MRI and CT do not require stress; they offer sensitivity and specificity similar to those of nuclear imaging; they achieve resolution better than that of nuclear imaging; and they can demonstrate the 3-dimensional (3D) coronary anatomy.
Therefore, MRI and CT complement the combination of stress test and catheterization, and in some settings, MRI and/or CT may replace them (eg, by demonstrating normal results).
EBT offers similar value. EBT is a form of CT in which an electron beam, rather than the entire x-ray source, is rotated around the patient. Also, EBT and CT have been used as a screening test to screen for calcifications in the coronary arteries as a marker for risk of coronary disease in young patients.
To monitor angiogenesis, collateral-sensitive and delayed-arrival MRI appear to be far more sensitive than any other technique. Collateral-sensitive MRI generates a dark flare of susceptibility effect due to sparse neovascular development at an early stage while suppressing a similar effect from the LV. This finding is a strong predictor (r = 0.93) of improved blood delivery.
Data from quantitative studies of the extent of delayed arrival in humans and from double-blind postmortem evaluations in porcine models of chronic myocardial ischemia and angiogenesis have validated this method.
This finding clearly distinguishes angiogenic treatment from control at 4 weeks after treatment, and the benefit is followed by improvements in wall motion (serial motion assessment by reference tracking [SMART] measurements).
Limitations of techniques
Coronary angiography is considered the criterion standard for evaluating coronary artery stenosis. Flow limitations may be estimated by using the TIMI (Thrombolysis in Myocardial Infarction)score and confirmed by using a flow wire or by performing IVUS.
If coronary angiography fails to depict a culprit lesion and if cardiac ischemia is inducible, the patient may have syndrome X (microvascular disease).
Coronary angiography requires the use of iodine, which may cause serious allergic reactions, including anaphylaxis and also renal failure. Use of large volumes of saline and the antioxidant acetylcysteine may help prevent renal failure. The catheterization procedure can induce vessel spasm and/or tear the lining of a vessel, resulting in occlusion and, possibly, death in a patient who may not have had coronary artery disease (CAD). The procedure can also result in embolism, which may cause stroke or limb loss. Nerve damage, infection, and other complications are possible as well. The death rate is approximately 0.1%.
Nuclear imaging produces low-resolution images that may depict an apparent defect resulting from breast tissue, hiccups, paradoxical septal motion, or other confounding factors. Nuclear imaging may fail to depict disease because of submaximal stress. Tomographic imaging, attenuation correction, or PET substantively eliminate the problems resulting from breast attenuation. The newer combinations of nuclear imaging with CT enable the most accurate correction of nuclear event maps for attenuation by overlying tissues.
MRI requires special precautions in patients with pacemakers or recently placed aneurysm clip. Patients with claustrophobia require premedication, mirrors, and/or an open magnet. Many magnets do not accommodate patients who weigh more than 300 lb. Arrhythmias commonly lower image quality.
CT contrast agents usually contain iodine, which may cause an allergic reaction and possibly anaphylaxis. Nonionic contrast material reduces the risk of harm, as does pretreatment with steroids. Gadopentetate dimeglumine, the contrast agent used for MRI, may be used for CT if patients are allergic to iodine-based media.
CT uses x-rays typically equivalent to the dose needed for about 200 chest radiographs. A single routine CT study in a child increases the lifetime risk of cancer by 0.35% per scan.
In adults, the lifetime risk of cancer may be as high as 2% with annual CT screening. Because the breast has high radiosensitivity, techniques to reduce tissue exposure, such as displacing the breasts outside the direct x-ray beam and using a lead shield, can reduce radiation hazard of CTA.
According to the 2015 update of the European procedural guidelines for radionuclide myocardial perfusion imaging (MPI) with SPECT, absolute contraindications for iodine contrast include myasthenia gravis, mastocytosis, and post-thyroid carcinoma when follow-up with 131I imaging or 131I therapy is planned within 6 months of CT angiography.
Risk factors that may warrant preadministration serum creatinine screening in patients who are scheduled to receive intravascular iodinated contrast medium include the following
:
Age >60 yr
History of renal disease, including dialysis, kidney transplant, single kidney, renal cancer, renal surgery
History of hypertension requiring medical therapy
Diabetes mellitus
The use of contrast media for cardiac imaging is increasing as hybrid cardiac SPECT/CT and PET/CT, as well as coronary CT angiography and cardiac MRI, become more widely used. Hybrid imaging provides a noninvasive assessment of coronary anatomy and myocardial perfusion.
Imaging guidance of interventional procedures
Coronary angiography is widely used to guide interventions, such as balloon angioplasty, atherectomy, laser treatment, stent placement, and other procedures. Current practice indicates the use of coronary angiography in patients with potentially treatable lesions to confirm the findings and to perform interventions. Both tasks may be accomplished in a single procedure.
Cardiac catheterization is recommended for patients with mild angina (class I or II) plus an EF of less than 45%, including patients with noninvasive test results indicating a high risk, those with an uncertain diagnosis after noninvasive testing, patients with serious ventricular arrhythmias, and those who survive an episode of sudden death. The only indication with submaximal support is mild angina with reduced EF; this is a class IIa recommendation. The classification of indications by the American College of Cardiology indicates the weight of evidence in support of the recommendation. Mild angina with no reduction in EF might be managed with medication as a therapeutic trial.
As an experiment, MRI, CT, or echocardiography may be used to guide interventional procedures. MRI does not involve ionizing radiation; therefore, imaging may be active throughout the procedure. However, special guidewires and other equipment compatible with the magnet and the rapidly changing magnetic field must be used, and staff must be trained to ensure that no magnetic objects are brought near the magnet.
CT uses ionizing radiation and is slower than coronary angiography, but it provides 3D information that may facilitate localization, especially for newer interventions such as the intramyocardial injection of angiogenic growth factors or stem cells. 3D ultrasonography similarly facilitates accurate injections, with convenience of portability and without a need for lead shielding from x-rays.