Practice Essentials
Spinal stenosis is a progressive narrowing of the spinal canal that occurs most commonly in the cervical and lumbar areas.
The prevalence of lumbar spinal stenosis is about 9.3%, with people in their 60s and 70s most commonly affected.
The incidence of spinal disease and the number of associated spinal operations has been documented to have increased in those populations that are increasingly aging.
Consensus criteria are needed to define and classify spinal stenosis. The means by which spinal stenosis is diagnosed is also changing. Concerns related to radiation risk of CT scans and the recognized limitations of spinal radiography suggest that MRI represents the best imaging modality. In many cases, clinical correlation between the findings on MRI and the symptomatic presentation of patients has been confirmed.
MRI helps avoid myelography and is often better accepted by patients who wish to avoid the associated (small) risk and pain associated with myelography. In selected patients, following placement of metallic fixation devices, myelography together with advanced CT techniques remains necessary. In one study, electrodiagnostic studies showed no superior accuracy as compared to MRI. Electrodiagnostic studies, when needed, should be limited to specific conditions such as radiating leg pain.
In a study comparing CT and MRI reliability, CT overestimated the degree of stenosis 20-35% of the time, and MRI overestimated the degree of stenosis 2-11% of the time.
Central spinal stenosis most commonly results from a developmental or degenerative narrow spinal canal. In certain cases, the spinal pedicles are shorter than normal. This is more common in the lumbar spine. Recognition of this primary defect in patients with short pedicles has led to pedicle-lengthening osteotomy as a treatment.
In some cases, spinal stenosis may be caused by spinal tumors such as a meningioma or the less common osteochondroma.
Because of the variable causes of spinal stenosis, imaging of the spine remains central to the diagnosis and the pre- and post-surgical management of the patient with symptomatic back pain.
Spinal stenosis rates and the money spent to treat spinal stenosis and back pain have increased. In addition to the generally increasing age of the population, many theories have been offered regarding the increased occurrence, with obesity being considered as the most likely factor.
Preferred examination
The selection of an initial screening examination in patients who are suspected of having spinal stenosis depends on the age of the patient. Older patients in whom spinal stenosis is suspected should be examined initially using conventional spinal radiographic imaging. Cervical stenosis assessment in older patients should include anteroposterior (AP), lateral, oblique, and swimmer’s lateral views. AP and lateral views of the thoracic spine are most useful for those patients at risk of a compression fracture. The lateral view of the thoracic spine assists in the evaluation of kyphosis. Assessment of the lumbar spine should include a lower lumbar centered, AP, lateral, and oblique projections. Lateral views are most sensitive for central spinal stenosis, whereas oblique views of the cervical and lumbar areas better demonstrate lateral stenosis syndromes. In older patients, radiography of the cervical, thoracic, and lumbar spine have value for screening for compression fractures or spondylosis. If the patient is symptomatic with radiculopathy or weakness or altered gate, MRI of the spine is the preferred method. CT of the spine should be limited to trauma and to those patients who have contraindications for MRI.
Younger patients and all patients in whom conventional radiology findings are negative should be evaluated using either spinal CT scanning with multiplanar reformatted images or spinal MRI. MRI of the spine is the more sensitive and specific study and is preferred in most cases. CT of the spine remains the primary means of diagnosis in cases of acute trauma. Nuclear medicine, including single-photon emission computed tomography (SPECT) bone scintigraphy, is generally reserved for the presumptive evaluation of infections, metastatic and primary neoplasms, and complex occult trauma. The amount of radiation exposure to patients should be carefully monitored, especially in the case of children and young adults.
In cases that require additional investigation following radiographs or CT, spinal MRI is the most universally suitable technique for the diagnosis of spinal stenosis. The examination should be performed using thin sections (3 mm) and high resolution (256 × 192 matrices). Spinal MRI should include imaging sets obtained in the axial and sagittal planes using T1-weighted, proton-density, and T2-weighted fast spin-echo and gradient-echo techniques. In cases that may involve bone marrow edema, T2-weighted STIR images are highly sensitive in the detection of marrow edema. The bony and osteophytic components of the spinal stenosis pattern are seen best using a T2-weighted gradient-echo technique.
CT scanning of the cervical, thoracic, and/or lumbar spine may be necessary for certain patients, often during the performance of CT myelography. CT myelography with thin CT scan images and multiplanar reconstructions offers excellent visualization of the neuro foraminal spaces and improved understanding of the degree of central canal stenosis. Indications for CT myelography include contraindications for MRI, implanted metal devices, and postoperative suggested complications. CT scanning of the spine should be followed by multiplanar reformatted images and 3-dimensional (3D) imaging techniques in selected patients.
CT and MRI studies in patients who are asymptomatic and younger than 40 years demonstrate a 4-28% occurrence of spinal stenosis. Most persons older than 60 years have spinal stenosis to some degree. Progressive narrowing of the spinal canal may occur alone or in combination with acute disc herniations. Close clinical correlation to MRI examinations of the spine has shown a close correlation between the incidence rate of neurologic deficits with the degree of changes in the spine, as visualized by MRI.
Nuclear medicine’s SPECT bone scintigraphy is valuable primarily in differentiating spondylosis with stenosis from medical disease, infections, and tumors.
The goal of spinal imaging is to localize the site and level of disease and to help differentiate between conditions in which patients require surgery and conditions in which patients recover following conservative treatment. It is important to correlate imaging findings with the signs and symptoms of the spinal disease under consideration. It is also important to compare prior examinations to current studies whenever possible. Spinal stenosis is generally a progressive condition that should be followed with a linear point of view based on prior examinations.
Limitations of techniques
Radiography of the spine is insensitive for detection of spinal stenosis based on changes in soft tissues of the spine. Superimposed structures and body habitus often limit the accuracy of measurements of the spinal canal.
CT scanning of the spine without IV contrast provides excellent detail of the bony tissues and some information about central soft-tissue abnormalities. The use of intravenous contrast agents improves the soft-tissue resolution of CT significantly. The use of intrathecal contrast as a CT myelogram introduces some increased risk of injury, a low risk of infection, and added expense; however, in patients who have had metallic anterior or posterior fixation procedures, CT myelography remains an essential alternative diagnostic method.
MRI provides excellent soft-tissue differentiation but has somewhat limited spatial resolution compared to CT. MRI contrast agents further improve soft-tissue visualization but have no effect on spatial resolution. The definition of cortical bone lesions and fractures is less with MRI than with CT. The incidence of failed or unsatisfactory MRI examinations due to motion, claustrophobia, and other technical incidents is higher with MRI than with CT.
SPECT bone scintigraphy is sensitive to diseases that actively affect bone pathophysiology, but spatial resolution is limited. Positive results are more likely for lesions that have osteoblastic activity.
Discography remains a controversial imaging technique that has limited or no application in the diagnosis of central spinal canal stenosis.
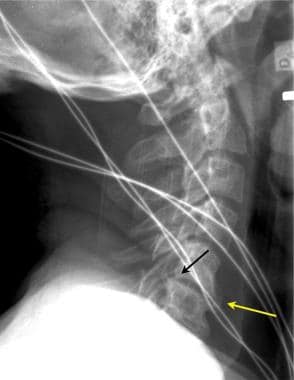
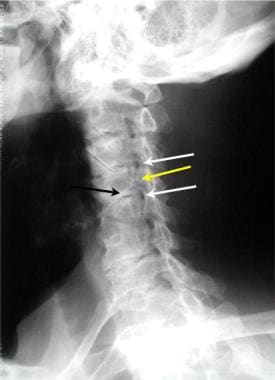
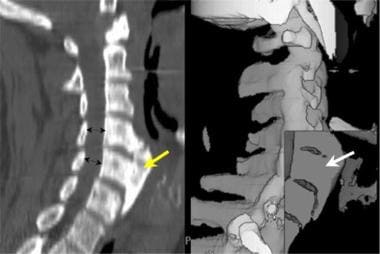
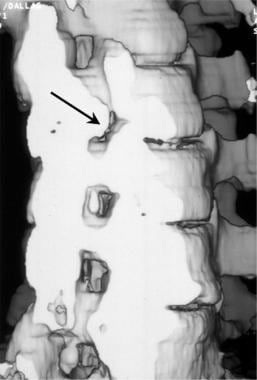
See the images below displaying spinal stenosis.
Lateral cervical spine radiographs may demonstrate significant degenerative changes with both interspace narrowing (yellow arrow) and osteophytic spinal canal narrowing (black arrow) in otherwise asymptomatic patients. This lateral radiographic film was taken for the evaluation of trauma. The patient had no chronic neurologic complaints.
To better evaluate the lower cervical spine, a lateral view of the cervical spine with the patient’s right arm above the head (swimmer’s view) may be helpful. In this case of trauma, the lower cervical spine (vertebral level C6/C7) was seen in the lateral projection only on the swimmer’s view (white arrow). Note the cervical spondylosis, which was an incidental finding.
Oblique view of the cervical spine demonstrates 2 levels of foraminal stenosis (white arrows) resulting from facet hypertrophy (yellow arrow) and uncovertebral joint hypertrophy.
This midline sagittal multireformatted computed tomography scan of the cervical spine (left image) demonstrates a very large anterior osteophyte (yellow arrow) that is causing dysphasia. The spinal canal is normal in diameter (black double arrows). The shaded surface volume image of the same patient (right image) demonstrates the uniformly dense nature of the hypertrophic bone in this patient (white arrow).
Sagittal volume reconstruction of a computed tomography scan of cervical spinal stenosis. The reconstructed image has been cut along the midline sagittal plane to demonstrate the spinal canal. Note the large central osteophyte (black arrow) at the C3/C4 vertebral level, which narrows the anteroposterior diameter of the cervical spine.
Oblique 3-dimensional shaded surface display computed tomography reconstruction of right foraminal stenosis resulting from unilateral facet hypertrophy (black arrow). The volume of the reconstruction has been cut obliquely across the neuroforaminal canal.
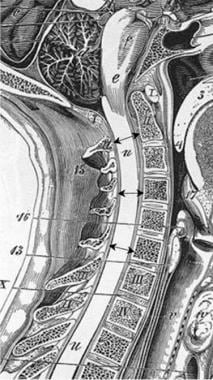
Anatomy
The AP diameter of the normal adult male cervical canal has a mean value of 17-18 mm at vertebral levels C3-5 (see the image below). The lower cervical canal measures 12-14 mm. Cervical stenosis is associated with an AP diameter of less than 10 mm, whereas diameters of 10-13 mm are relatively stenotic in the upper cervical region.
Sagittal measurements taken of the anteroposterior diameter of the cervical spinal canal are highly variable in otherwise healthy persons. An adult male without spinal stenosis has a diameter of 16-17 mm in the upper and middle cervical levels. Magnetic resonance imaging (MRI) scans and reformatted computed tomography (CT) images are equally as effective in obtaining these measurements, whereas radiography is not accurate.
In the central cervical spinal region, hypertrophy of the ligamentum flavum, bony spondylitic hypertrophy, and bulging of the disc annulus contribute to development of central spinal stenosis. In each case, the relative significance of each structure contributing to the stenosis is variable.
Movement of the cervical spine exacerbates congenital or acquired spinal stenosis. In hyperextension, the cervical cord increases in diameter while posterior ligaments have been shown to buckle or fold, increasing the risk of spinal cord compression. Within the canal, the anterior roots are pinched between the annulus margins and spondylotic bony bars that form along the disc-vertebral margins and arise from uncovertebral joint hypertrophy. In the posterior canal, hypertrophic facet joints and thickened infolded ligamentum flavum compress the dorsal nerve roots. In hyperflexion, neural structures are tethered anteriorly against the bulging disc annulus and spondylotic bars. In the event of a vertebral collapse, the cervical spine loses its shape, which may result in anterior cord compression.
In cases of severe central cervical spinal stenosis, the possibility of thoracic or lumbar stenosis should be carefully considered. Stenotic cauda equina syndrome has been reported after surgical decompression of cervical stenosis.
Lateral cervical stenosis results from encroachment on the lateral recess and the neuroforamina of the cervical region, primarily as a result of hypertrophy of the uncovertebral joints, lateral disc annulus bulging, and facet hypertrophy.
The thoracic spinal canal varies from 12 to 14 mm in diameter in the adult. Primary central thoracic spinal stenosis is rare. Occasionally, hypertrophy or ossification of the posterior longitudinal ligament results in central canal stenosis. Thoracic spinal symptoms require careful consideration of primary spinal cord lesions. The occurrence of other levels of spinal stenosis in patients who present with thoracic myelopathy is high.
A full spinal evaluation is recommended for the patient who presents with thoracic myelopathy. This can most easily be performed as a whole spine MRI protocol using a wider field to include the entire spine in a study that is acceptable to the patient.
Lateral thoracic stenosis may result from hypertrophy of facet joints with occasional synovial cyst encroachment.
The AP diameter of the normal lumbar spinal canal varies widely from 15 to 27 mm. Lumbar stenosis results from an AP spinal canal diameter of less than 12 mm in some patients; a diameter of 10 mm is definitely stenotic and may be a primary source of symptoms.
Differentials and other problems to be considered
The differential diagnosis of spinal stenosis includes many conditions, including congenital conditions such as achondroplasia and osteogenesis imperfecta . Degenerative conditions such as osteoporosis and osteogenetic arthritis are common. Inflammatory diseases may include rheumatoid arthritis of the spine and spondylodiskitis. Other conditions to be considered include metastatic breast cancer, prostate cancer, and Paget disease.
Certain diseases and conditions such as Morquio syndrome manifest spinal stenosis as a major cause of morbidity.
Radiologic intervention
Uncomplicated spinal stenosis is not typically treated using interventional radiologic techniques. Pain management, including facet injections, may provide temporary relief for patients; however, if the underlying pattern of stenosis results in nerve root compression with edema or spinal cord compression, surgical management may be necessary. Biopsy of metastatic spinal disease is performed easily using CT scan guidance to aid in the diagnosis. Spinal stenosis associated with compression fractures has been successfully treated using percutaneous kyphoplasty and percutaneous vertebroplasty.
As the population ages, the frequency and severity of spinal stenosis are likely to continue to increase. Attempts have been made to developm less invasive means of treating spinal stenosis and the related pain.
Minimally invasive spinal fusion using bilateral transforaminal lumbar interbody fusion for high-grade isthmic defects has been reported.
Other percutaneous interventions, including adhesiolysis, have been reported.
Nonsurgical pain management techniques may provide relief from pain following failed back surgery.
Medicolegal pitfalls
The surgical introduction of pedicle screws and intervertebral disc space implants may be associated with injury to nerve roots and, rarely, the spinal cord. Postoperative patients should be carefully evaluated for hardware failure, mistaken introduction, and migration. Subdural hemorrhage has been reported during spinal decompression surgery.