Overview
Diffuse axonal injury (DAI) is a frequent result of traumatic acceleration/deceleration or rotational injuries and a frequent cause of persistent vegetative state in patients. In fact, DAI represents approximately one half of all intra-axial traumatic lesions.
This lesion is the most significant cause of morbidity in patients with traumatic brain injuries, which most commonly result from high-speed motor vehicle accidents. Any patient with a closed head injury who experiences extensive loss of consciousness and neurological deficits warrants neuroimaging.
Diffuse axonal injury typically consists of several focal white-matter lesions measuring 1-15 mm in a characteristic distribution.
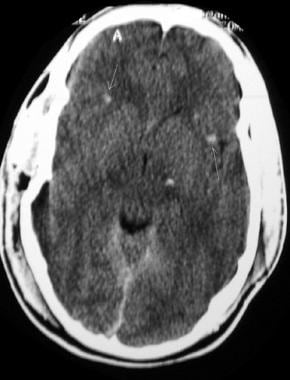
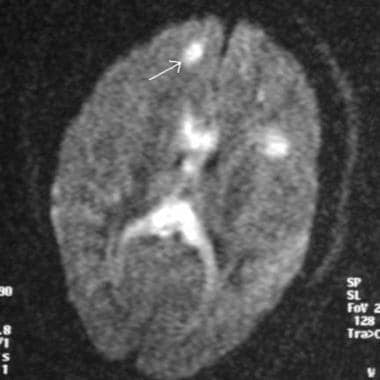
See the images below.
Noncontrast computed tomography scan of a trauma patient demonstrates multiple petechial hemorrhages (arrows) consistent with diffuse axonal injury. Note that the hemorrhages are characteristically located at the gray-white matter interface.
Magnetic resonance imaging diffusion sequence demonstrating multiple foci of abnormal increased signal at the gray-white matter junction (arrow) and within the corpus callosum in a patient with diffuse axonal injury
Classically, DAI has been considered a primary-type injury, with damage occurring at the time of the accident. Research has shown that another component of the injury comprises the secondary factors (or delayed component), since the axons are injured, secondary swelling occurs, and retraction bulbs form. Of patients with DAI, 80% demonstrate multiple areas of injury on computed tomography (CT) scans.
The degree of microscopic injury usually is considered to be greater than that seen on diagnostic imaging, and the clinical findings reflect this point. DAI is suggested in any patient who demonstrates clinical symptoms disproportionate to his or her CT-scan findings. DAI results in instantaneous loss of consciousness, and most patients (>90%) remain in a persistent vegetative state, since brainstem function typically remains unaffected. DAI rarely causes death.
Preferred Examination
Magnetic resonance imaging (MRI) is the preferred examination for DAI (particularly with gradient-echo sequences), although CT scanning may demonstrate findings suggestive of DAI and is more practical and available.
Studies have indicated that MRI can play a role in predicting the length of coma in DAI patients. However, MRI is contraindicated in patients with implanted pacemakers or certain types of metallic prostheses, as well as in patients who have metallic foreign bodies, such as bullet fragments, in their head or neck or near important vascular structures. In addition, MRI is difficult to perform on patients who have claustrophobia and on ventilator-dependent patients.
Traumatic microbleeds are considered to be a radiologic marker for DAI. Gradient echo-sequence-based susceptibility-weighted imaging has been found to be sensitive and accurate for microbleed detection.