Practice Essentials
Raynaud phenomenon manifests as recurrent vasospasm of the fingers and toes and usually occurs in response to stress or cold exposure.
The phenomenon is named for Maurice Raynaud, who, as a medical student, defined the first case in 1862 as “episodic, symmetric, acral vasospasm characterized by pallor, cyanosis, suffusion, and a sense of fullness or tautness, which may be painful.”
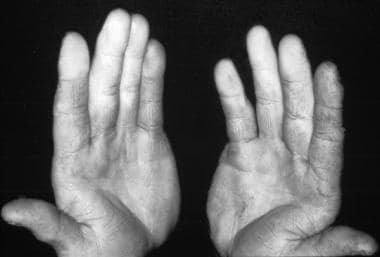
See the image below.
Photo of a patient with Raynaud phenomenon that resulted from working with a jackhammer. Courtesy of the CDC.
See Cutaneous Clues to Accurately Diagnosing Rheumatologic Disease, a Critical Images slideshow, to help recognize cutaneous manifestations of rheumatologic diseases.
Secondary Raynaud phenomenon should be distinguished from primary Raynaud phenomenon (Raynaud disease). They are distinct disorders that share a similar name. Raynaud disease is characterized by the occurrence of the vasospasm alone, with no association with another illness. Secondary Raynaud phenomenon is a designation usually used in the context of vasospasm associated with another illness, most commonly an autoimmune disease.
Diagnostic criteria for primary Raynaud phenomenon include the following
:
Attacks triggered by exposure to cold and/or stress
Symmetric bilateral involvement
Absence of necrosis
Absence of a detectable underlying cause
Normal capillaroscopy findings
Normal laboratory findings for inflammation
Absence of antinuclear factors
Young women who have had Raynaud phenomenon alone for more than 2 years and have not developed any additional manifestations are at low risk for developing an autoimmune disease. The same should not be said for older patients and male patients with Raynaud phenomenon, as vasospastic symptoms may predate systemic disease by as many as 20 years. In some studies, 46%-81% of affected patients have secondary Raynaud phenomenon.
Although Raynaud phenomenon has been described with various autoimmune diseases, the most common association is with progressive systemic sclerosis (90% in individuals with scleroderma) and mixed connective-tissue disease (85% prevalence). Raynaud phenomenon has also been described with such diverse diseases as systemic lupus erythematosus and other disorders not classified as autoimmune, including frostbite, vibration injury, polyvinyl chloride exposure, and cryoglobulinemia.
For primary Raynaud phenomenon, the first line of therapy consists of lifestyle measures. If these prove inadequate, the patient may benefit from pharmacologic treatment. Therapy for secondary Raynaud phenomenon must be tailored to the underlying disorder. Patients with secondary Raynaud phenomenon are more likely to require pharmacologic therapy. A variety of drugs are used off-label for treatment; the most commonly used drug is nifedipine. See Treatment and Medication.
For discussion of Raynaud phenomenon in children, see Pediatric Raynaud Phenomenon.