Recovery Considerations
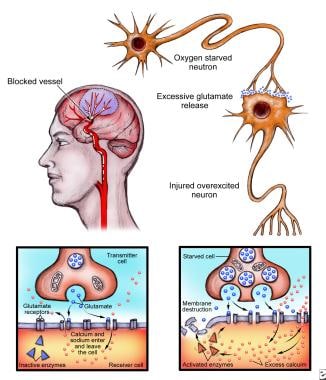
Stroke rehabilitation is a combined and coordinated use of medical, social, educational, and vocational measures to retrain a person who has suffered a stroke to his/her maximal physical, psychological, social, and vocational potential, consistent with physiologic and environmental limitations. The cellular mechanisms behind stroke are seen in the image below.
When the brain suffers an injury, such as a stroke, neurons release glutamate onto nearby neurons, which become excited and overloaded with calcium, after which they die (left). Normal neurotransmission (above) is altered during injury, causing excess calcium to activate enzymes, eventually leading to destruction of the cell. Since this process occurs via glutamate receptors, including N-Methyl-D-aspartate (NMDA) receptors, scientists believe that damage can be stopped through the use of agents that block these receptors.
Evidence from clinical trials supports the premise that early initiation of therapy favorably influences recovery from stroke. When the initiation of therapy is delayed, patients may in the interim develop avoidable secondary complications, such as contractures and deconditioning.
In addition, many studies show that stroke rehabilitation can improve functional ability even in patients who are elderly or medically ill and who have severe neurologic and functional deficits.
The initial clinical examination of a patient with an acute stroke includes a thorough, detailed neurologic examination. The neurologic findings are used by the rehabilitation team for prognostication, development of the specific details of the rehabilitation plan, and selection of the appropriate setting for rehabilitation.
Reassessment of the patient’s condition during rehabilitation provides a means of monitoring progress and subsequently evaluating outcome. The initial rehabilitation assessment should begin immediately following onset, within 2-7 days, and then subsequently at repeated intervals.
Go to Stroke, Ischemic, for more complete information on this topic.
Timing, extent, and types of recovery
Patients recover after stroke in 2 different, but related, ways.
A reduction in the extent of neurologic impairment can result from spontaneous, natural neurologic recovery (via the effects of treatments that limit the extent of the stroke) or from other interventions that enhance neurologic functioning. A patient demonstrating this form of recovery presents with improvements in motor control, language ability, or other primary neurologic functions.
The second type of recovery demonstrated by stroke patients is the improved ability to perform daily functions within the limitations of their physical impairments. A patient who has sensorimotor, cognitive, or behavioral deficits resulting from stroke may regain the capacity to carry out activities of daily living (ADL), such as feeding himself/herself, dressing, bathing, and toileting, even if some degree of residual physical impairment remains.
The ability to perform these tasks can improve through adaptation and training in the presence or absence of natural neurologic recovery, which is thought to be the element of recovery on which rehabilitation exerts the greatest effect.
Hemiparesis and motor recovery have been the most studied of all stroke impairments. As many as 88% of patients with acute stroke have hemiparesis.
In a classic report, Twitchell described in detail the pattern of motor recovery following stroke.
At onset, the upper extremity (UE) is more involved than the lower extremity (LE), and eventual motor recovery in the UE is less than in the LE. The severity of UE weakness at onset and the timing of the return of movement in the hand are important predictors of eventual motor recovery in the UE. A systematic review of 58 studies confirms the most important predictive factor for upper limb recovery following stroke is the initial severity of motor impairment or function.
The prognosis for return of useful hand function is unfavorable when UE paralysis is complete at onset or grasp strength is not measurable by 4 weeks.
However, as many as 9% of patients with severe UE weakness at onset may gain good recovery of hand function. As many as 70% of patients showing some motor recovery in the hand by 4 weeks make a full or good recovery. Full recovery, when it occurs, usually is complete within 3 months of onset.
Bard and Hirshberg asserted that if no initial motion is noticed during the first 3 weeks or if motion in one segment is not followed within a week by the appearance of motion in a second segment, the prognosis for recovery of full motion is not favorable.
Although most recovery from stroke takes place in the first 3 months, and only minor additional measurable improvement occurs after the 6 months following onset, recovery may continue over a longer period of time in some patients who have significant partial return of voluntary movement.
Criteria for admission to a comprehensive rehabilitation program
Criteria for a patient’s admission to a comprehensive rehabilitation program may include the following:
Stable neurologic status
Significant persisting neurologic deficit
Identified disability affecting at least 2 of 5 functions, including mobility, self-care activities, communication, bowel or bladder control, and swallowing
Sufficient cognitive function to learn
Sufficient communicative ability to engage with therapists
Physical ability to tolerate the active program
Achievable therapeutic goals