Practice Essentials
Blastomycosis is a systemic pyogranulomatous infection usually caused by the inhalation of (spores) conidia of Blastomyces dermatitidis. Clinical presentations vary widely, ranging from an asymptomatic, self-limited pulmonary infection to acute respiratory distress syndrome (ARDS), a life-threatening disease.
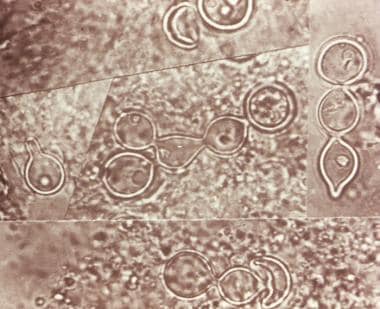
Composite photomicrograph of a tissue specimen from a patient with blastomycosis infection shows an abundance of large budding cells that had been configured in chains. Courtesy of CDC/Dr. Lucille K. George.
Signs and symptoms
Blastomycosis is usually localized to the lungs and may present with:
A self-limited flulike illness with fever, chills, myalgia, headache, and a nonproductive cough
An acute illness resembling bacterial pneumonia, with high fever, chills, a productive cough, and pleuritic chest pain; mucopurulent or purulent sputum
Chronic illness, with low-grade fever, a productive cough, fatigue, night sweats, and weight loss
Rapidly progressive, and severe disease (eg, multilobar pneumonia or ARDS), with fever, shortness of breath, tachypnea, hypoxemia and, finally, hemodynamic collapse
Extrapulmonary manifestations are present in 25-40% of patients, who may present with:
Cutaneous lesions – Usually either verrucous or ulcerative and may be asymptomatic
Osteoarticular lesions – Cause bone or joint pain; possible soft-tissue swelling; possible involvement of any bone, but the vertebrae and pelvis are common sites
Genitourinary manifestations including prostatitis and epididymitis – May be asymptomatic or may cause pain on urination
Other sites – B dermatitidis has been reported to involve almost all organs, including the eye, liver, spleen, breast, thyroid, and adrenal gland.
Central nervous system involvement – Intracranial or epidural abscesses and meningitis
See Presentation for more detail.
Diagnosis
Culture and cytopathology are the gold standard for the diagnosis of blastomycosis. The fastest way to diagnose blastomycosis is direct identification of the broad based budding yeast forms under microscopy. Identification from culture may not be evident for 2 to 4 weeks, and it often requires invasive procedures such as bronchoscopy or tissue biopsy to obtain specimens.
More recently, molecular DNA probes have been developed to facilitate the rapid identification of B dermatitidis from clinical specimens. A commercially available chemiluminescent DNA probe assay (AccuProbe) is commonly used and produces results from culture within hours once there is adequate growth.
In addition, tests targeting virulence factors BAD1 and DRK1 through real-time polymerase chain reaction (RT-PCR) and serologic antibody-based assays have been developed but are as yet not commercially available.
Chest imaging findings are nonspecific and may range from scattered centrilobular nodules to areas of dense consolidation. Computed tomography (CT) scanning is not always necessary, but it can provide better definition of the character and distribution of abnormalities observed on a chest radiograph.
See Workup for more detail.
Management
Antifungal treatment is as follows:
Patients with mild to moderate pulmonary disease – Oral azole (eg, itraconazole)
Patients with moderate-to-severe disseminated disease or immune compromise: Initially, amphotericin B with step-down to an oral azole after clinical improvement
Patients with central nervous system (CNS) disease as well as pregnant women: Always be treat initially with amphotericin B
See Treatment and Medication for more detail.