Practice Essentials
Obstructive sleep apnea (OSA)—also referred to as obstructive sleep apnea-hypopnea—is a sleep disorder that involves cessation or significant decrease in airflow in the presence of breathing effort. It is the most common type of sleep-disordered breathing and is characterized by recurrent episodes of upper airway collapse during sleep.
These episodes are associated with recurrent oxyhemoglobin desaturations and arousals from sleep.
OSA that is associated with excessive daytime sleepiness is commonly called obstructive sleep apnea syndrome—also referred to as obstructive sleep apnea-hypopnea syndrome.
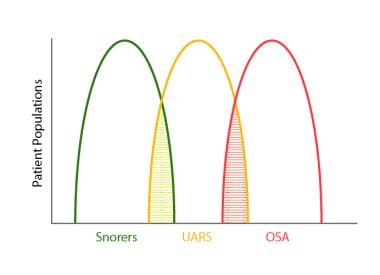
The image below illustrates the sleep-related disordered breathing continuum ranging from simple snoring to OSA.
Sleep-related disordered breathing continuum ranging from simple snoring to obstructive sleep apnea (OSA). Upper airway resistance syndrome (UARS) occupies an intermediate position between these extremes. Note areas of overlap among the conditions.
Signs and symptoms
Generally, symptoms of OSA begin insidiously and are often present for years before the patient is referred for evaluation.
Nocturnal symptoms may include the following:
Snoring, usually loud, habitual, and bothersome to others
Witnessed apneas, which often interrupt the snoring and end with a snort
Gasping and choking sensations that arouse the patient from sleep, though in a very low proportion relative to the number of apneas they experience
Nocturia
Insomnia; restless sleep, with patients often experiencing frequent arousals and tossing or turning during the night
Daytime symptoms may include the following:
Nonrestorative sleep (ie, “waking up as tired as when they went to bed”)
Morning headache, dry or sore throat
Excessive daytime sleepiness that usually begins during quiet activities (eg, reading, watching television); as the severity worsens, patients begin to feel sleepy during activities that generally require alertness (eg, school, work, driving)
Daytime fatigue/tiredness
Cognitive deficits; memory and intellectual impairment (short-term memory, concentration)
Decreased vigilance
Morning confusion
Personality and mood changes, including depression and anxiety
Sexual dysfunction, including impotence and decreased libido
Gastroesophageal reflux
Hypertension
See Clinical Presentation for more detail.
Diagnosis
In general, the physical examination is normal in patients with OSA, aside from the presence of obesity (body mass index: >30 kg/m2), an enlarged neck circumference (men: >43 cm [17 in]; women: >37 cm [15 in]), and hypertension.
Evaluate the upper airway in all patients, particularly in nonobese adults with symptoms consistent with OSA.
Examination findings may include the following:
Abnormal (increased) Mallampati score: Identifies risk for difficult tracheal intubation
Narrowing of the lateral airway walls: Independent predictor of the presence of obstructive sleep apnea in men but not women
Enlarged (ie, “kissing”) tonsils (3+ to 4+)
Retrognathia or micrognathia
Large degree of overjet
High-arched hard palate
Systemic arterial hypertension: Present in about 50% of obstructive sleep apnea cases
Congestive heart failure
Pulmonary hypertension
Stroke
Metabolic syndrome
Type 2 diabetes mellitus
Testing
An overnight sleep study, or polysomnography, is required to diagnose OSA.
Routine laboratory tests, however, are usually not helpful in OSA unless a specific indication is present. Pulmonary function tests are not indicated to make a diagnosis of, or treatment plan for, OSA alone. The standard indications for such testing apply to all patients, with or without OSA.
Obtain a thyrotropin test on any patient with possible OSA who has other signs or symptoms of hypothyroidism, particularly in elderly individuals.
AASM standards and guidelines for diagnostic polysomnography
The American Academy of Sleep Medicine guidelines for the indications and performance of polysomnography include the following
:
Sleep stages are recorded via an electroencephalogram, electro-oculogram, and chin electromyogram
Heart rhythm is monitored with a single-lead electrocardiogram
Leg movements are recorded via an anterior tibialis electromyogram
Breathing is monitored, including airflow at the nose and mouth (using both a thermal sensor and a nasal pressure transducer), effort (using inductance plethysmography), and oxygen saturation
The breathing pattern is analyzed for the presence of apneas and hypopneas (as per definitions standardized by the American Academy of Sleep Medicine)
See Workup for more detail.
Management
Treatment of OSA partly depends on the patients’ severity of sleep-disordered breathing. Those with mild apnea have more options, whereas people with moderate to severe apnea should be treated with nasal continuous positive airway pressure (CPAP).
Conservative therapy and prevention
The following conservative measures may help manage or prevent OSA:
Restriction of body positions during sleep (avoid supine position)
Sleeping in an upright position for markedly obese patients
Avoiding smoking; smoking cessation
Avoiding alcohol and other sedatives (particularly 4-6 hours before bedtime)
Avoiding sleep deprivation
Mechanical measures
Mechanical measures used in the treatment of OSA include the following:
Nasal CPAP: Standard treatment option
Bilevel positive airway pressure
Oral appliance therapy
Pharmacotherapy
Medications are generally not a part of the primary treatment recommendations for OSA. However, central nervous system stimulants (eg, modafinil, armodafinil) or solriamfetol (a dopamine/norepinephrine reuptake inhibitor) may be considered for adjunctive use to treat excessive daytime sleepiness in the management of this condition.
Surgery
Surgical intervention for OSA includes, but is not limited to, the following:
Uvulopalatopharyngoplasty
Craniofacial reconstruction with advancement of tongue or maxillomandibular bones
Tracheostomy
See Treatment and Medication for more detail.