Practice Essentials
Many histologic tumor types present in the skull base. The skull base can be divided into the anterior, middle, and posterior compartments or fossae. The skull base is a highly complex region that includes multiple bones. Eleven pairs of cranial nerves and the olfactory nerves (CN I) pass through the inner table of the skull via 7 pairs of bony foramina and the cribriform plate (CN I). The skull base also has multiple foramina that provide passage for vascular and other neural elements. The anatomy relevant to surgery greatly varies and depends on the location of the tumor and adjacent skull base structures. Primary tumors may derive from the bone, paranasal sinuses, nasopharynx, inner ear, dura, cranial nerves, and brain. These lesions cause symptoms through mass effect or through the invasion of local structures. Metastatic tumors also present in the skull base and may produce mass effect or invade adjacent tissue.
Skull base tumors include the following: meningiomas, pituitary tumors, sellar/parasellar tumors, vestibular and trigeminal schwannomas, esthesioneuroblastomas, chordomas, and chondrosarcomas.
Surgical approaches for skull base tumors include the following: modified orbitozygomatic, pterional, middle fossa, retrosigmoid, far lateral craniotomy, and midline suboccipital craniotomy.
Skull base tumors can be classified based on their tissue of origin, histologic characteristics, and common anatomic locations. Unfortunately, even benign lesions may cause progressive and unrelenting deficits if located in an area where complete resection is not allowed and growth cannot be controlled with medical or radiation therapy.
The anatomic location of a lesion often presents a significant challenge for safe surgical access because of the proximity or involvement of critical neural and vascular structures and the need to preserve the barrier between the cerebrospinal fluid (CSF) and the external environment. Tumors and surgical approaches are classified based on the involved area. The development of brain exposing osteotomies, endoscopic surgery, infection prevention methods (eg, galeal, frontalis, and myofascial flaps), and improved techniques for reconstruction allow surgeons to perform biopsies and resections on most skull base masses. In addition, radiosurgery has become a highly useful tool in treating pathologic conditions at the skull base. As expertise with surgical approaches to the skull base has grown, the optimal application of these methods in combination with adjuvant therapies has become the focus of skull base neurosurgery.
The symptoms and life expectancy of the patient, natural history of the disease, and structures involved by the tumor all must be considered before recommending treatment. In many cases, biopsy helps determine the diagnosis. A larger craniotomy for extensive resection may then be recommended. In patients who harbor aggressive malignant lesions, which often preclude surgical cure, biopsy can prevent the need for an extensive craniotomy. When craniotomy is undertaken, the goals of surgery are to minimize morbidity and to maximize the extent of tumor removal.
Contraindications to surgical correction of skull base tumors are based on the patient’s comorbidities and his or her ability to tolerate surgery. The poor long-term prognosis for patients with malignancy often overshadows the use of a large skull base resection in favor of a less-invasive palliative approach.
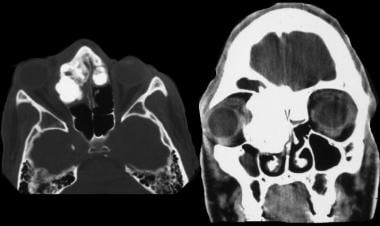
The image below depicts a CT scan revealing a skull base tumor.
Osteoma. CT scan with axial bone windows and coronal plane reconstruction that demonstrates a fibrous osteoma that involves the right orbit and the floor of the anterior cranial fossa.
Tumor types
Osteoma
Osteomas are the most common primary tumor of the bone of the calvaria.
They are benign growths of dense cortical bone. These tumors often arise from the paranasal sinuses but may develop in the frontal bone (arising from the area of the frontal sinus), cranial vault, mastoid sinus, or mandible. These tumors grow slowly and rarely expand internally to compress the brain; therefore, they are usually asymptomatic. Osteomas have been associated with Gardner syndrome, an autosomal-dominant variant of familial adenomatous polyposis, which consists of multiple cranial osteomas, colonic polyposis, and soft-tissue tumors.
Chondroma
Chondromas are rare, slow-growing tumors that arise from the cartilaginous portion of bones formed by enchondral ossification. In the cranial region, this includes the bones of the skull base and paranasal sinuses. Progression to a malignant chondrosarcoma (see Chondrosarcoma below) is rare.
Hemangioma
Hemangiomas of the skull are benign vascular bone tumors composed of cavernous or capillary vascular channels. Skull hemangiomas vary from small to very large and may be solitary or multiple. They make up approximately 7% of skull tumors. There are 2 types, the more common cavernous hemangioma and the more rare capillary hemangioma.
Dermoid and epidermoid tumors of the skull
Dermoid and epidermoid tumors are benign lesions of the skull that develop in the cranial vault, paranasal sinuses, orbit, and petrous bone. They are among the most common benign skull lesions in children. These tumors usually arise in the midline, in the diploe of the bone, where they expand both the inner and outer tables of the skull.
Plasmacytoma plasma cell tumors
Plasmacytoma plasma cell tumors tumors are monoclonal expansions of immunoglobulin-secreting plasma cells and may present as solitary benign bone tumors called plasmacytomas (see the image below). Intracranial plasmacytoma is rare.
Disseminated disease is known as multiple myeloma and carries a much less favorable prognosis than solitary plasmacytoma. Solitary intracranial plasmacytoma of the skull base carries a dissemination rate of up to 100%, which is considerably higher than the rate associated with intracranial plasmacytoma of the dura or convexities.
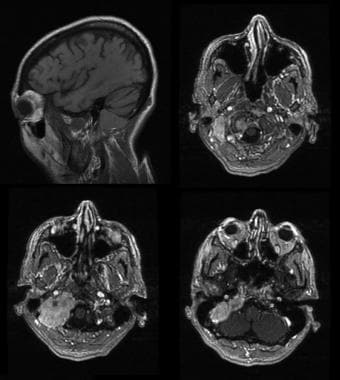
Intracranial plasmacytoma. Sagittal and axial T1-weighted MRI with contrast enhancement demonstrate a right-sided plasmacytoma of the petrous bone. This tumor was treated through a far lateral approach and suboccipital craniotomy following a superselective embolization of feeding arteries.
Paragangliomas
Paragangliomas, such as glomus jugulare tumors, are benign neuroendocrine tumors that arise from chromaffin cells in the bony canals of temporal bone. These tumors are rare and represent 0.6% of all head and neck tumors; they present with a female-to-male ratio of 6:1.
Paragangliomas are locally invasive, and approximately 40% expand into the posterior cranial fossa, where they are identified as lesions of the cerebellopontine angle.
They rarely spread distally or involve the lymph nodes.
Larger tumors may cause symptoms related to cerebellar and brain stem compression. Functional tumors represent the 1-3% of paragangliomas that produce catecholamines; the remainder are considered nonfunctional. Those that secrete catecholamines may cause a life-threatening cardiac arrhythmia or hypertensive emergency.
Other benign skull tumors
Other benign lesions that affect bone and sometimes involve the skull include aneurysmal bone cysts, osteoid osteoma, ossifying and nonossifying fibromas, and some variants of giant cell tumors. Bony involvement is best demonstrated on CT scan with bone windows. MRI can demonstrate intracranial extension.
Chondrosarcoma
Chondrosarcoma is a malignant cartilage tumor that originates from enchondral bones. It is composed of cartilage-producing cells. It makes up 0.15% of intracranial tumors and 6% of skull base tumors.
When it develops in the skull base, it usually arises in the parasellar area, cerebellopontine angle, or paranasal sinuses. It may also arise in the clivus (see the image below). It is most common in men in the fourth decade of life. Skull base lesions are thought to arise from the persistent islands of embryonal cartilage that occur near the cranial base synchondroses.
Clival chondrosarcoma. Contrast-enhanced T1-weighted MRI in the coronal plane. This tumor involved the clivus and posterior clinoid and encroached on the optic chiasm in the suprasellar region. It was subtotally resected through a frontotemporal craniotomy with a zygomatic osteotomy.
Chondrosarcomas can be divided into conventional, clear cell, mesenchymal, and dedifferentiated variants. When located in the skull base, the conventional pattern is most common. Conventional chondrosarcomas have been further subdivided into histologic grades I-III. The lower-grade tumors are less aggressive and have minimal malignant potential. These tumors do not stain for epithelial markers or oncofetal antigens, distinguishing them from chordomas (see below). Low-grade classic chondrosarcomas generally carry a good prognosis. They commonly present with cranial nerve palsies such as diplopia, hoarseness, dysphagia, facial dysesthesia, hearing loss, headache, and gait disturbance. They are overall slow growing, but they are locally aggressive.
Chordoma
Chordoma is a low-grade malignancy that arises from tissue of the primitive notochord (in normal development becomes the nucleus pulposus of the intervertebral disk).
Approximately 40% of these tumors arise in the clivus (see the image below), with the remainder developing along the vertebral axis, most commonly in the sacrococcygeal region. Chordomas may develop in persons of any age, but they manifest most commonly in persons aged 20-40 years. A slight male predominance exists.
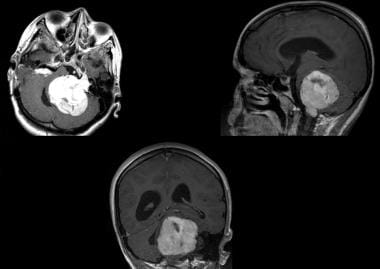
Chordoma. T1-weighted MRI with contrast that demonstrates an enhancing mass that replaced the clivus and invaded the right cavernous sinus. This lesion was subtotally resected using a sublabial approach. The patient was then treated with gamma knife radiosurgery (GKRS).
Clival chordoma is locally invasive and may extend into the middle fossa or brainstem. It recurs despite surgical resection and radiotherapy and may destroy surrounding tissues, but it rarely metastasizes. Chordomas are usually extradural in origin. Dural invasion is possible but usually develops late in the course of aggressive tumors or with recurrent tumors if a dural defect was left after the initial operation.
Microscopically, chordomas have a lobular arrangement of physaliferous cells, containing large vacuoles and mucus. These cells are surrounded by abundant extracellular mucoid tissue. Approximately 10% of chordomas show more malignant histologic features, which are sometimes related to previous irradiation.
Osteogenic sarcoma and fibrous sarcoma
Osteogenic sarcoma (osteosarcoma) is the most common malignant primary tumor of bone. It develops most frequently in the second decade of life and may be associated with prior radiation, Paget disease, fibrous dysplasia (see the image below), or chronic osteomyelitis.
Fibrous dysplasia. Coronal reconstruction of nonenhanced CT scan that demonstrates fibrous dysplasia of the right orbit with extension into the floor of the anterior fossa. This lesion was completely resected using a multidisciplinary team and a craniofacial approach that included a bifrontal craniotomy
Nerve sheath tumors
Intracranial nerve sheath tumors grow at the skull base, where cranial nerves exit the brain stem and approach the bony foramina. These lesions develop sporadically or as part of the genetic syndromes neurofibromatosis-1 (NF-1) and neurofibromatosis-2 (NF-2). Sporadic cases generally manifest as a single lesion, whereas multiple tumors present as part of a hereditary syndrome.
The most common intracranial nerve sheath tumors are schwannomas. These lesions arise almost exclusively from sensory nerves. The most common is the vestibular schwannoma (sometimes called acoustic neuroma; see the images below). Much less common are the trigeminal schwannoma and hypoglossal schwannoma (see the images below). Schwannomas and neurofibromas are well encapsulated and can usually be completely resected, although the involved nerve must often be sacrificed. The malignant peripheral nerve sheath tumor is infiltrating and highly aggressive and therefore cannot be cured with excision.
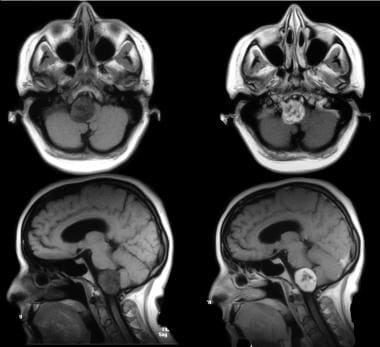
Vestibular schwannoma. T1-weighted MRI scan that demonstrates a large left-sided vestibular schwannoma in a 19-year-old woman with neurofibromatosis type II. Also present on the left is a vagal (tenth nerve) schwannoma. A residual tumor from a right-sided vestibular schwannoma, which was previously operated on, is visible. These lesions were resected through a retrosigmoid approach and suboccipital craniectomy.
Hypoglossal schwannoma. Precontrast (left) and Postcontrast (right) T1-weighted MRI scans that demonstrate a right-sided schwannoma of the hypoglossal (XII) nerve. This tumor was completely resected using an extreme lateral approach and suboccipital craniectomy.
Vestibular schwannoma (acoustic neuroma, acoustic neurofibroma) is a benign tumor that arises from Schwann cells of the vestibular branch of the VIII nerve in more than 90% of cases; less than 10% arise from the cochlear branch of VIII. Vestibular schwannoma accounts for 5-10% of all intracranial tumors and is the most common tumor of the cerebellopontine angle. The peak age for tumor occurrence is between age 40 and 60 years, and they are twice as common in women as in men. Bilateral tumors occur in less than 5% of patients and, when present, are diagnostic for NF-2 (see the image below).
Vestibular schwannoma. T1-weighted MRI scan that demonstrates a large left-sided vestibular schwannoma in a 19-year-old woman with neurofibromatosis type II. Also present on the left is a vagal (tenth nerve) schwannoma. A residual tumor from a right-sided vestibular schwannoma, which was previously operated on, is visible. These lesions were resected through a retrosigmoid approach and suboccipital craniectomy.
Vestibular schwannomas grow slowly into the internal auditory meatus and the cerebellopontine angle, displacing the adjacent cerebellum, pons, or cranial nerves (usually V and VII). Because they grow slowly, many tumors are large and even cystic before they become symptomatic. The growth rate may increase during pregnancy.
Trigeminal schwannomas account for less than 8% of intracranial schwannomas and less than 0.4% of all intracranial tumors.
They originate within the ganglion, nerve root, or 1 of the 3 divisions of the trigeminal nerve. About 50% of these tumors are limited to the middle fossa, while 30% extend into the posterior fossa and 20% are dumbbell-shaped and extend into both fossae. Diagnosis is best established with MRI. The differential diagnosis includes meningioma, vestibular schwannoma, epidermoid lesions, and primary bone tumors of the skull base.
Malignant peripheral nerve sheath tumors are a rare and aggressive type of spindle cell tumor. They affect patients primarily aged 20-50 years. They originate from perineural or Schwann cells of the peripheral nerve sheath. They can present as a painless, progressively enlarging, subcutaneous mass.
Meningioma
Meningiomas arise from meningothelial cells, which are most common in the arachnoid villi, and they comprise 22% of all intracranial tumors. They account for 3-12% of cerebellopontine angle tumors. Most meningiomas are diagnosed in the sixth or seventh decades of life. They are more common in women, with a female-to-male ratio of 3-2:1. Five to fifteen percent of patients with meningiomas have multiple meningiomas (see the images below), especially those with NF-2. More than 90% of tumors are intracranial and 10% intraspinal.
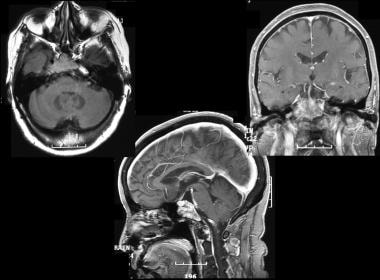
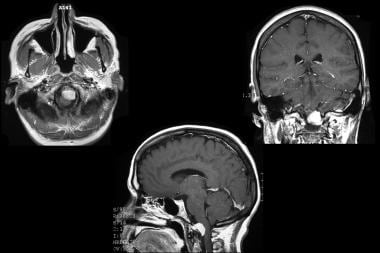
Foramen magnum meningioma. Contrast-enhanced T1-weighted MRI scans that demonstrate a ventral, left-sided meningioma at the foramen magnum. This tumor was completely resected using a far lateral approach and suboccipital craniotomy with C1 laminectomy.
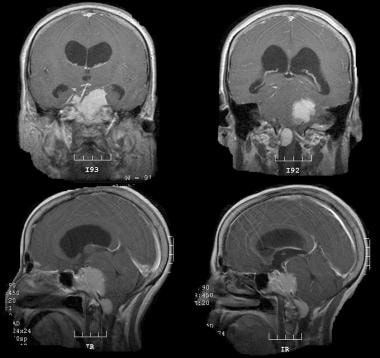
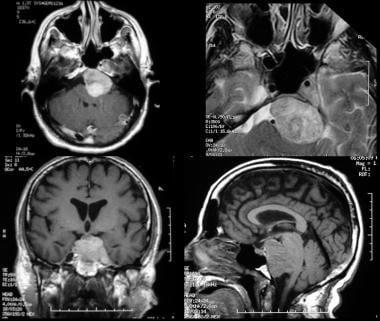
Multiple skull base meningiomas. Contrast-enhanced T1-weighted MRI in the coronal (above) and sagittal (below) planes demonstrates a large left-sided petroclival meningioma and a right-sided meningioma at the foramen magnum. After shunt placement to treat hydrocephalus, the petroclival tumor was resected using a presigmoid approach. The foramen magnum tumor was subsequently resected.
The only proven nongenetic risk factor for meningioma formation is radiation exposure. Radiation-induced meningiomas tend to develop over the cerebral convexities rather than at the skull base. Trauma has been suggested as a risk factor for meningioma formation and may be involved in the formation of intraosseous meningiomas, which can present at the skull base.
Almost all familial meningiomas develop within the context of NF-2, and patients with NF-2 are at increased risk for meningiomas as well as vestibular schwannomas. These patients often have multiple tumors of both varieties. Deletion of the c-sis protooncogene (a polypeptide homologous with platelet-derived growth factor [PDGF] receptor) on chromosome 22 has been linked to meningioma formation. Abnormalities in other chromosomes suggest that several oncogenes or tumor suppressor genes are involved in meningioma formation.
Most meningiomas are nodular and compress adjacent structures. Occasionally, they are distributed in sheathlike formations (meningioma en plaque). This pattern is especially common in skull base meningiomas of the sphenoid ridge (see the images below). All meningiomas are encapsulated and attach to the dura, from which they derive their blood supply. Hyperostosis of the underlying bone is common and can be appreciated radiographically.
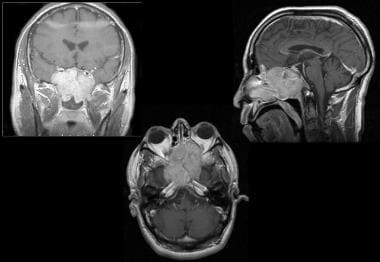
Right sphenoid wing meningioma with intraorbital involvement. Contrast-enhanced T1-weighted sagittal MRI scan. This tumor manifested as slowly progressive unilateral vision loss and mild proptosis on the right. It was resected using a frontotemporal craniotomy with orbitozygomatic osteotomy. Note the right sphenoid hyperostosis, which is best seen on the axial image.
Right sphenoid wing meningioma with intraorbital involvement. Contrast-enhanced T1-weighted axial MRI scan. This tumor manifested as slowly progressive unilateral vision loss and mild proptosis on the right side. It was resected using a frontotemporal craniotomy with orbitozygomatic osteotomy. Note the right sphenoid hyperostosis.
The World Health Organization grading system classifies meningiomas as typical (or benign), atypical, or malignant based on cellularity, cytologic atypia, mitosis, and necrosis. Malignant meningiomas are rare but aggressive, and about half metastasize systemically, usually in bone, liver, or lung. Benign meningiomas recur in about 7-20% of patients, atypical variants recur in 29-40% of patients, and anaplastic tumors recur in 50-78% of patients. Brain invasion may develop with all 3 histological grades of meningioma. Brain invasion connotes a greater likelihood of recurrence but does not indicate a truly malignant histologic pattern. Nevertheless, an elevated proliferation index (>5%) does predict a poor outcome.
The most common histologic subtypes of meningioma include meningotheliomatous (syncytial), fibrous, transitional, and psammomatous. Clinically, these subtypes are of little value, but select subtypes have prognostic relevance. Clear-cell meningiomas make up 0.2-0.81% of all meningiomas and are often more aggressive than more common varieties, with frequent recurrence and CNS metastasis.
Secretory meningiomas secrete vascular endothelial growth factor (VEGF) and are associated with extensive edema.
Papillary or rhabdoid meningioma variants must be treated as malignant tumors.
Hemangiopericytoma
Hemangiopericytoma is a rare lesion that comprises 0.4% of primary CNS tumors. It is a richly vascular and highly cellular tumor that is almost invariably associated with the meninges. They are a type of sarcoma that derives from pericytes that surround blood vessels. They often appear much like meningiomas on imaging.
A hemangiopericytoma is also more likely to recur than typical meningioma and systemic metastasis is possible.
Specific tumor locations
Tumors of the skull base may also be described on the basis of their most common presenting location. Tumor location often dictates the presenting signs and symptoms. The skull base can be divided into the anterior, middle and posterior fossae. This distinction helps the surgeon choose which surgical approach offers the greatest opportunity for complete tumor removal with minimal potential for neurologic injury.
Tumors of the anterior cranial fossa
The tumors of the anterior cranial fossa may be malignant or benign. The malignant tumors in this group include tumors that arise in the nasal cavity and paranasal sinuses (eg, juvenile angiofibroma, esthesioneuroblastoma [see the image below], inverted papilloma, lymphoma, nasopharyngeal carcinoma). Other malignant tumors that develop in this region include orbital gliomas and other orbital tumors, rhabdomyosarcomas, and osteogenic sarcomas. The benign tumors that develop specifically in the anterior skull base include ossifying fibromas.
Esthesioneuroblastoma. A 39-year-old man presented with 1 month of decreased vision, left facial numbness, and swelling. Physical examination demonstrated left-sided exophthalmos and blindness. He was also unable to smell. Contrast-enhanced T1-weighted MRI demonstrated a large lesion that originated in the paranasal sinuses and extended through the cribriform plate into the anterior cranial fossa. He underwent a bifrontal craniotomy for resection of this tumor.
Several of the malignant tumors unique to the anterior skull base are rare entities. Esthesioneuroblastoma, also termed olfactory neuroblastoma, is a very rare tumor. Nasopharyngeal carcinoma is the most common skull base lesion that requires multidisciplinary surgical management. These tumors may enter the intracranial space by extension through the cribriform plate. Histologic variants of nasopharyngeal carcinoma include squamous cell carcinoma and adenoid cystic carcinoma (see the images below).
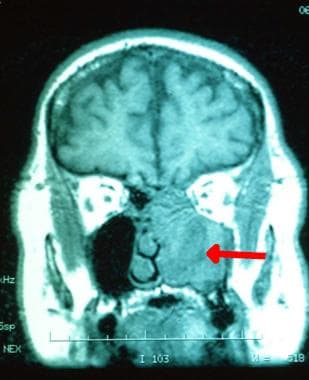
Adenoid cystic carcinoma. A T1-weighted image from an MRI scan that demonstrates a tumor (red arrow) that involves the ethmoid sinuses and cribriform plate.
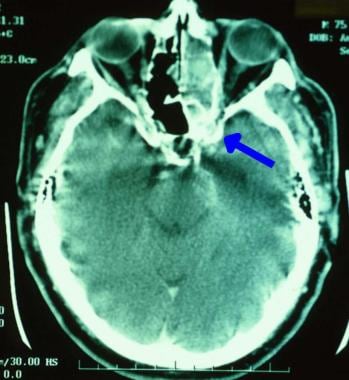
Adenoid cystic carcinoma. Extension of the tumor into the middle fossa anterior to the temporal lobe (blue arrow).
Tumors of the middle cranial fossa
Tumors unique to the middle cranial base are usually benign. These tumors include pituitary adenomas, craniopharyngiomas, cavernous sinus meningiomas, temporal bone tumors, cholesteatomas, and enchondromas. Malignant tumors in this area may arise primarily (chondrosarcoma [see the image below] and osteogenic sarcoma) or secondarily through local invasion or hematologic spread from distant sites.
Clival chondrosarcoma. Contrast-enhanced T1-weighted MRI in the coronal plane. This tumor involved the clivus and posterior clinoid and encroached on the optic chiasm in the suprasellar region. It was subtotally resected through a frontotemporal craniotomy with a zygomatic osteotomy.
Meningiomas of the cavernous sinus present a unique challenge because resection is likely to damage multiple cranial nerves. In young patients with no ocular muscle palsy, some authors recommend subtotal resection and radiotherapy.
Tumors of the posterior cranial fossa
Tumors unique to the posterior cranial fossa include both benign and malignant lesions. Malignant tumors are discussed further below (see Malignancy and Metastasis, below). Benign tumors that specifically involve the posterior skull base include meningiomas of the foramen magnum, clivus and cerebellopontine angle, epidermoids, dermoids, chondromas, and chordomas (see the images below).
Foramen magnum meningioma. Contrast-enhanced T1-weighted MRI scans that demonstrate a ventral, left-sided meningioma at the foramen magnum. This tumor was completely resected using a far lateral approach and suboccipital craniotomy with C1 laminectomy.
Multiple skull base meningiomas. Contrast-enhanced T1-weighted MRI in the coronal (above) and sagittal (below) planes demonstrates a large left-sided petroclival meningioma and a right-sided meningioma at the foramen magnum. After shunt placement to treat hydrocephalus, the petroclival tumor was resected using a presigmoid approach. The foramen magnum tumor was subsequently resected.
Petroclival meningioma. Contrast-enhanced T1-weighted and a T2-weighted (upper right) MRI scan that demonstrates a large left-sided petroclival meningioma. This tumor was near totally resected using a presigmoid approach. The patient subsequently underwent gamma knife radiosurgery (GKRS) for the treatment of the residual tumor.
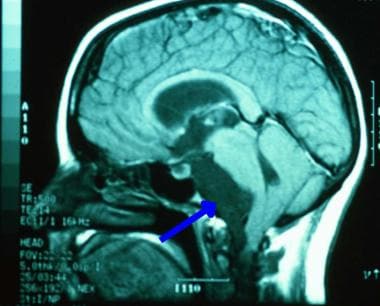
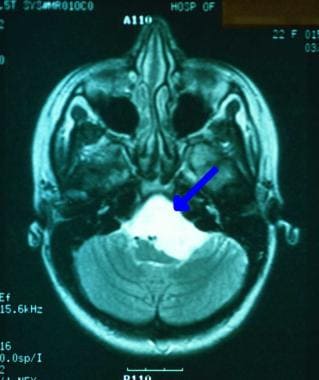
Skull base tumors. Sagittal enhanced T1-weighted image from an MRI scan that shows a hypointense mass (blue arrow) anterior to the brainstem.
Skull base tumors. Axial T2-weighted image from an MRI scan that demonstrates a hyperintense mass (blue arrow) anterior to and compressing the brainstem.
Chordoma. T1-weighted MRI with contrast that demonstrates an enhancing mass that replaced the clivus and invaded the right cavernous sinus. This lesion was subtotally resected using a sublabial approach. The patient was then treated with gamma knife radiosurgery (GKRS).
Clivus meningiomas arise anterior to the brainstem. Lateral extension into the petrous bone may complicate surgery because of cranial nerve involvement. Clear-cell meningiomas are also most commonly found in the posterior fossa.
Foramen magnum meningiomas cause pain, gait difficulties, and wasting of the hand muscles. They are intimately entwined with the cranial nerves, complicating complete resection.
Malignancy and metastasis
Metastasis to the skull base
Malignant tumors that involve the skull base are less common than their benign counterparts. Their aggressive nature and tissue of origin, often adjacent to the intracranial vault, merit a unique approach to their surgical management. As the cranial nerves exit the bony foramina of the skull, they are vulnerable to entrapment and compression by osseous metastasis. Skull base metastases usually arise from a prostate, breast, lung, or head and neck primary lesion or from lymphoma. The cardinal sign of metastatic skull base invasion is cranial neuropathy, which is typically sudden in onset. Although skull base metastases are often painless, localized cranial or facial pain at the site of tumor invasion may be a symptom.
MRI scans can reveal even small skull base metastases. Almost all tumors can be visualized, especially if they lie within the cavernous sinus. Empiric treatment without histologic documentation may be indicated when symptoms are progressive, the clinical picture is clear, and biopsy is difficult or hazardous.
Direct extension of malignant tumors to the skull base
Several malignant tumors involve the base of the skull by direct extension. These include squamous cell carcinoma (of the nasal sinuses and temporal bone), adenoid cystic carcinoma (of the salivary glands; see the images below), esthesioneuroblastoma (of the olfactory mucosa; see the image below), and nasopharyngeal carcinoma.
Adenoid cystic carcinoma. A T1-weighted image from an MRI scan that demonstrates a tumor (red arrow) that involves the ethmoid sinuses and cribriform plate.
Adenoid cystic carcinoma. Extension of the tumor into the middle fossa anterior to the temporal lobe (blue arrow).
Esthesioneuroblastoma. A 39-year-old man presented with 1 month of decreased vision, left facial numbness, and swelling. Physical examination demonstrated left-sided exophthalmos and blindness. He was also unable to smell. Contrast-enhanced T1-weighted MRI demonstrated a large lesion that originated in the paranasal sinuses and extended through the cribriform plate into the anterior cranial fossa. He underwent a bifrontal craniotomy for resection of this tumor.
These tumors affect cranial nerve function, but unlike metastases, they often also cause pain. Imaging demonstrates erosion of the skull base and the presence of a soft tissue mass; biopsy is diagnostic. Small tumors can sometimes be cured with wide surgical excision before they invade sensitive neural structures. However, most tumors are more extensive when detected, and despite treatment with radical excision and radiation therapy, the prognosis is often poor.