Practice Essentials
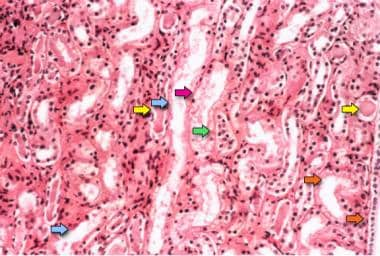
Acute kidney injury (AKI) is defined as an abrupt or rapid decline in renal filtration function. See the image below.
Photomicrograph of a renal biopsy specimen shows renal medulla, which is composed mainly of renal tubules. Features suggesting acute tubular necrosis are the patchy or diffuse denudation of the renal tubular cells with loss of brush border (blue arrows); flattening of the renal tubular cells due to tubular dilation (orange arrows); intratubular cast formation (yellow arrows); and sloughing of cells, which is responsible for the formation of granular casts (red arrow). Finally, intratubular obstruction due to the denuded epithelium and cellular debris is evident (green arrow); note that the denuded tubular epithelial cells clump together because of rearrangement of intercellular adhesion molecules.
Signs and symptoms
Skin
Skin examination may reveal the following in patients with AKI:
Livedo reticularis, digital ischemia, butterfly rash
Palpable purpura: systemic vasculitis
Maculopapular rash: Allergic interstitial nephritis
Track marks (ie, intravenous drug abuse): Endocarditis
Eyes
Eye examination may reveal the following:
Keratitis, iritis, uveitis, dry conjunctivae: Autoimmune vasculitis
Jaundice: Liver diseases
Band keratopathy (ie, hypercalcemia): Multiple myeloma
Signs of diabetes mellitus
Signs of hypertension
Atheroemboli: Retinopathy (ie, Hollenhorst plaque in cholesterol microembolism)
Ear
Examination of the patient’s ears may reveal the following signs:
Hearing loss: Alport disease and aminoglycoside toxicity
Mucosal or cartilaginous ulcerations: granulomatosis with polyangiitis (Wegener granulomatosis)
Cardiovascular system
Cardiovascular examination may reveal the following:
Irregular rhythms (ie, atrial fibrillation): Thromboemboli
Murmurs: Endocarditis
Pericardial friction rub: Uremic pericarditis
Increased jugulovenous distention, rales, S
3: Heart failure
Abdomen
The following signs of AKI may be discovered during an abdominal examination:
Pulsatile mass or bruit: Atheroemboli
Abdominal or costovertebral angle tenderness: Nephrolithiasis, papillary necrosis, renal artery thrombosis, renal vein thrombosis
Pelvic, rectal masses; prostatic hypertrophy; distended bladder: Urinary obstruction
Limb ischemia, edema: Rhabdomyolysis
Pulmonary system
Pulmonary examination may reveal the following:
Rales: pulmonary edema, infectious pulmonary process
Hemoptysis: ANCA vasculitis, anti–glomerular basement membrane (anti-GBM, Goodpasture) syndrome
See Presentation for more detail.
Diagnosis
The following tests can aid in the diagnosis and assessment of AKI:
Kidney function studies: Increased levels of blood urea nitrogen (BUN) and creatinine are the hallmarks of renal failure; the ratio of BUN to creatinine can exceed 20:1 in conditions that favor the enhanced reabsorption of urea, such as volume contraction (this suggests prerenal AKI)
Complete blood count (can indicate infection; acute blood loss or chronic anemia; thrombotic microangiopathy)
Peripheral smear (eg, schistocytes such as hemolytic-uremic syndrome and thrombotic thrombocytopenic purpura)
Serologic tests: These may show evidence of conditions associated with AKI, such as in lupus nephritis, ANCA vasculitis or anti-GBM disease or syndrome
Complement testing: Pattern may indicate AKI related to endocartis or various glomerulonephritidites
Fractional excretion of sodium and urea in the setting of oliguria
Bladder pressure: Patients with a bladder pressure above 25 mm Hg should be suspected of having AKI caused by abdominal compartment syndrome
Ultrasonography: Renal ultrasonography is useful for evaluating existing renal disease and obstruction of the urinary collecting system
Aortorenal angiography : Can be helpful in establishing the diagnosis of renal vascular diseases, such as renal artery stenosis, renal atheroembolic disease, atherosclerosis with aortorenal occlusion, and certain cases of necrotizing vasculitis (eg, polyarteritis nodosa)
Renal biopsy: Can be useful in identifying intrarenal causes of AKI and directing targeted therapy
See Workup for more detail.
Management
Maintenance of volume homeostasis and correction of biochemical abnormalities remain the primary goals of AKI treatment and may include the following measures:
Correction of fluid overload with furosemide
Correction of severe acidosis with alkali administration, which can be important as a bridge to dialysis
Correction of life-threatening hyperkalemia
Correction of hematologic abnormalities (eg, anemia, uremic platelet dysfunction) with measures such as RBC or platelet transfusions and administration of desmopressin or estrogens
Dietary changes are an important facet of AKI treatment. Restriction of salt and fluid becomes crucial in the management of oliguric renal failure, in which the kidneys do not adequately excrete either toxins or fluids.
Pharmacologic treatment of AKI has been attempted on an empiric basis, with varying success rates.
See Treatment and Medication for more detail.
For patient education information, see Acute Kidney Failure.