Practice Essentials
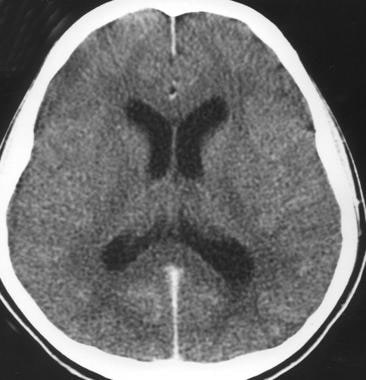
Meningitis is a clinical syndrome characterized by inflammation of the meninges. The image below depicts acute bacterial meningitis.
Acute bacterial meningitis. This axial nonenhanced computed tomography scan shows mild ventriculomegaly and sulcal effacement.
Signs and symptoms
The classic triad of bacterial meningitis consists of the following:
Fever
Headache
Neck stiffness
Up to 95% of patients with bacterial meningitis have at least two of the four following symptoms: fever, headache, stiff neck, or altered mental status.
Other symptoms can include nausea, vomiting, photalgia (photophobia), sleepiness, confusion, irritability, delirium, and coma. Patients with viral meningitis may have a history of preceding systemic symptoms (eg, myalgias, fatigue, or anorexia).
The history should also address the following:
Epidemiologic factors and predisposing risks such as mosquito bites (West Nile virus in endemic months, June-October in the United States)
Exposure to a sick contacts (small children with febrile illness)
Previous medical treatment and existing conditions
Geographic location and travel history
Season and temperature (enterovirus and West Nile virus in the summer and fall; herpes simplex virus type 2 year round)
Acute bacterial meningitis in otherwise healthy patients who are not at the extremes of age presents in a clinically obvious fashion; however, subacute bacterial meningitis often poses a diagnostic challenge.
General physical findings in viral meningitis are common to all causative agents. Enteroviral infection is suggested by the following:
Exanthemas
Contact with small children with febrile illnesses
Symptoms of pericarditis, myocarditis, or conjunctivitis
Syndromes of pleurodynia, herpangina, and hand-foot-and-mouth disease
Infants may have the following:
Bulging fontanelle (if euvolemic)
Paradoxic irritability (ie, remaining quiet when stationary and crying when held)
High-pitched cry
Hypotonia
The examination should evaluate the following:
Focal neurologic signs
Signs of meningeal irritation
Systemic and extracranial findings
Level of consciousness
In chronic meningitis, it is essential to perform careful general, systemic, and neurologic examinations, looking especially for the following:
Lymphadenopathy
Papilledema
Meningismus
Cranial nerve palsies
Other focal neurological signs
Patients with aseptic meningitis syndrome usually appear clinically nontoxic, with no vascular instability. They characteristically have an acute onset of meningeal symptoms, fever, and CSF pleocytosis that is usually prominently lymphocytic.
See Clinical Presentation for more detail.
Diagnosis
The diagnostic challenges in patients with clinical findings of meningitis are as follows:
Early identification and treatment of patients with acute bacterial meningitis
Assessing whether a treatable CNS infection is present in those with suspected subacute or chronic meningitis
Identifying the causative organism
Blood studies that may be useful include the following:
Complete blood count (CBC) with differential
Serum electrolytes
Serum glucose (which is compared with the CSF glucose)
Blood urea nitrogen (BUN) or creatinine and liver profile
In addition, the following tests may be ordered:
Blood, nasopharynx, respiratory secretion, urine or skin lesion cultures or antigen/polymerase chain reaction (PCR) detection assays
Syphilis testing
Serum procalcitonin testing
Lumbar puncture and CSF analysis
Neuroimaging (CT of the head or MRI of the brain)
See Workup for more detail.
Management
Initial measures include the following:
Shock or hypotension – Crystalloids
Altered mental status – Seizure precautions and treatment (if necessary), along with airway protection (if warranted)
Stable with normal vital signs – Oxygen, IV access, and rapid transport to the emergency department (ED)
Treatment of bacterial meningitis includes the following:
Prompt initiation of empiric antibacterial therapy as appropriate for patient age and condition
After identification of the pathogen and determination of susceptibilities, targeted antibiotic therapy as appropriate for patient age and condition
Steroid (typically, dexamethasone) therapy
In certain patients, consideration of intrathecal antibiotics
The following systemic complications of acute bacterial meningitis must be treated:
Hypotension or shock
Hypoxemia
Hyponatremia
Cardiac arrhythmias and ischemia
Stroke
Exacerbation of chronic diseases
Most cases of viral meningitis are benign and self-limited, but in certain instances, specific antiviral therapy may be indicated, if available.
Other types of meningitis are treated with specific therapy as appropriate for the causative pathogen, as follows:
Fungal meningitis – Cryptococcal (amphotericin B, flucytosine, fluconazole), Coccidioides immitis (fluconazole, amphotericin B, itraconazole), Histoplasma capsulatum (liposomal amphotericin B, itraconazole), or Candida (amphotericin plus 5-flucytosine)
Tuberculous meningitis (isoniazid, rifampin, pyrazinamide, ethambutol, streptomycin)
Parasitic meningitis (amebic [Naegleria fowleri] or acanthamebic) – Variable regimens
Lyme meningitis (ceftriaxone; alternatively, penicillin G, doxycycline, chloramphenicol)
See Treatment and Medication for more detail.