Practice Essentials
Human papillomavirus (HPV) produces epithelial tumors of the skin and mucous membranes. The current classification system for HPV, which is based on similarities in genomic sequences, generally correlates with the 3 clinical categories applied to HPV infection:
Anogenital or mucosal (further subclassified as latent [asymptomatic], subclinical, or clinical)
Nongenital cutaneous
Epidermodysplasia verruciformis (see the images below)
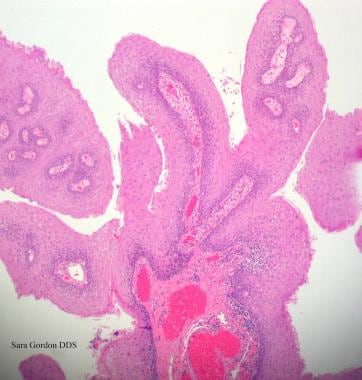
Human papillomavirus (HPV). Verrucae and papillomas appear as frondlike epithelial proliferations. Verrucae tend to be more keratinized with sharper projections than papillomas.
Human papillomavirus (HPV). Verruca vulgaris on the lateral border of the tongue exhibits the multiple, sharp-tipped, white, verrucous appearance, which is classic for this lesion in the oral cavity. Not all verrucae are so clinically diagnostic. Courtesy of Rose Yin Geist, DDS.
See Pediatric Vaccinations: Do You Know the Recommended Schedules?, a Critical Images slideshow, to help stay current with the latest routine and catch-up immunization schedules for 16 vaccine-preventable diseases.
Signs and symptoms
The clinical history and presentation of HPV infection vary according to the anatomic area involved. The predilection of certain viral genotypes for infecting certain epidermal sites largely determines areas of involvement. Conditions with which HPV is associated include the following:
Anogenital warts (condylomata acuminata): These are usually found near moist surfaces (eg, perianal area, vaginal introitus, vagina, labia, and vulva) but may also be found on dry surfaces (eg, penile shaft); they may be smooth and papular or keratotic; they generally are not painful but can be associated with pruritus or bleeding
Cervical disease (eg, low-grade squamous intraepithelial lesion [LGSIL] or high-grade squamous intraepithelial lesion [HGSIL])
Anal cancer: About 50% of men who are homosexual and have anal squamous cell carcinoma (SCC) have a history of anorectal warts; however, only 20% of women with SCC and men who are not homosexual have this history
Nonanogenital mucosal disease (eg, oral warts, respiratory papillomas, and focal epithelial hyperplasia [Heck disease])
Nongenital cutaneous disease (eg, common cutaneous warts [verruca vulgaris], flat warts [verruca plana] and Bowenoid papulosis)
Epidermodysplasia verruciformis
Physical findings vary, depending on the tissues involved, and may include the following:
Typical condylomata are discrete, papillary, cauliflower-like lesions that involve multiple sites on moist surfaces
Keratotic warts are often seen on dry surfaces such as the labia majora
Discrete papules 1-3 mm in size can present on the shaft of the penis
Cervical intraepithelial lesions may be found upon examination of the cervix
Subclinical infection may be present, with tiny, slightly raised areas felt or visualized on the vagina or cervix
See Clinical Presentation for more detail.
Diagnosis
The diagnosis of most cutaneous and external genital warts can be made through clinical examination or with application of acetic acid and biopsy. In genital intraepithelial neoplasia, it is essential to determine the extent of disease through careful inspection and colposcopy.
Laboratory studies that may be considered include the following:
Cervical cytologic testing with the Papanicolaou (Pap) test to screen for cervical neoplasia (guidelines for cervical cancer screening now include a delay in the initiation of screening and longer intervals between subsequent screens
)
HPV DNA testing (eg, with Hybrid Capture II or polymerase chain reaction [PCR] assay) for detection of HPV and posttreatment follow-up of cervical intraepithelial neoplasia
The acetic acid test: This test can be used in conjunction with colposcopy to examine cervical lesions; however, it is reserved for suspicious lesions and should not be used for routine screening
In some cases, tissue biopsy can be used to confirm HPV infection. A biopsy is recommended for the following scenarios:
Women with a history of vulvar dysplasia
Postmenopausal women
Women in whom medical therapy fails
Clinical doubt about the diagnosis
Histologic findings that can help elucidate the diagnosis include the following:
Common cutaneous warts: Marked hyperkeratosis, acanthosis, parakeratosis, and papillomatosis; warts can be distinguished from other papillomas by the presence of koilocytes, vertical columns of parakeratosis, and foci of clumped keratohyaline granules
Condyloma acuminatum: Disruption of the epidermis with hyperkeratosis, coarse keratohyaline granules, and koilocytes in a prominent granular layer; the epidermis or mucosa of flat condylomata demonstrates acanthosis
Bowenoid papulosis: Psoriasiform hyperplasia and hyperkeratosis of the epidermis, with increased mitotic figures at all epidermal levels and keratinocytes displaying enlarged pleomorphic and hyperchromic nuclei
See Workup for more detail.
Management
All medicines used to treat HPV disease are applied topically; they should not be applied to mucosal surfaces and should not be used to treat dysplastic lesions, squamous cell carcinoma, verrucous carcinoma, or Bowenoid papulosis. The following 2 broad categories of medications are effective:
Immune response modifiers (eg, imiquimod and interferon alfa): These are primarily used in treatment of external anogenital warts or condylomata acuminata
Cytotoxic agents: These include both antiproliferative drugs (eg, podofilox, podophyllin, and 5-fluorouracil [5-FU]) and chemodestructive or keratolytic agents (eg, salicylic acid, trichloroacetic acid [TCA], and bichloracetic acid [BCA]); the latter are the only agents recommended for treatment of nongenital cutaneous warts
Sinecatechins ointment is another option.
Surgical interventions are commonly considered when a large number of warts are present, a large area is affected, or the patient has refractory disease. Overall, physical destruction or excision has been more effective in eradicating genital warts than medical therapy. Primary surgical therapy can often be accomplished in the office and includes the following options:
Cryosurgery
Electrosurgery (electrodesiccation or a loop electrosurgical excision procedure [LEEP])
Simple surgical excision with a scalpel, scissors, or curette
Alternative surgical procedures include the following:
Carbon dioxide laser ablation
Cavitron Ultrasonic Surgical Aspiration (CUSA)
Mohs surgery
Vaccines are available for prevention of HPV infection, and recommended vaccination schedules have been outlined.
See Treatment and Medication for more detail.