Practice Essentials
Of the approximately 81,560 cases of non-Hodgkin lymphoma (NHL) expected to be diagnosed in 2021 in the United States,
approximately 20% are likely to be follicular lymphomas.
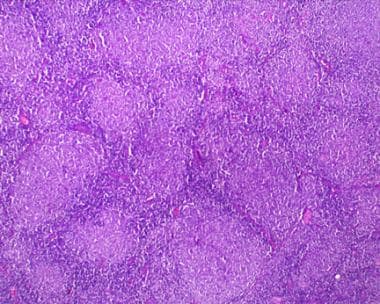
No sex preponderance is seen for follicular lymphomas, but the incidence increases with age and varies across racial groups. See the image below.
Follicular lymphoma, low-power view. Note the nodular pattern reminiscent of germinal centers. Photograph courtesy of Aamir Ehsan, MD.
Signs and symptoms
Follicular lymphoma is a type of non-Hodgkin lymphoma that most commonly presents as a painless, slowly progressive adenopathy. Systemic symptoms, such as fever, drenching night sweats, or weight loss in excess of 10% of ideal body weight, or asthenia, are infrequent at presentation but can be observed in later stages of the disease.
Symptoms related to bone marrow dysfunction, such as anemia, leukopenia, or thrombocytopenia, are rare at presentation but can also be observed in the later stages of the disease. Lymphocytosis, reflecting blood involvement, may also be present.
Despite the fact that most follicular lymphomas are advanced at the time of diagnosis, many patients may not require treatment for prolonged periods of time, and the median survival of patients with follicular lymphomas has historically been approximately 8-10 years.
Literature since the rituximab era has shown a further increase in overall survival.
Diagnosis
During the physical evaluation, all lymph node areas and the reticuloendothelial system should be examined. Involved nodes typically are nontender, firm, and rubbery in consistency. The throat, liver, and spleen should also be examined. Splenomegaly is present in approximately 50% of patients at presentation, and hepatosplenomegaly may occur.
A complete blood cell count (CBC) with differential should be obtained, including examination of the peripheral blood smear if the differential is abnormal. A chemistry panel and lactate dehydrogenase (LDH) level should be obtained.
A computed tomography (CT) scan of the chest, abdomen, and pelvis can determine whether abdominal or pelvic adenopathy is present. Positron emission tomography (PET) scanning may also be useful in certain clinical settings, such as localized disease or when transformed disease is suspected.
Biopsy is essential to establish a diagnosis of lymphoma. Obtain an excisional biopsy (or, if that is not possible, a core biopsy) of an involved node. If the disease is extranodal, a surgical biopsy sample should be obtained from the involved organ.
Because the chromosomal t(14;18) translocation is found in the majority of patients with follicular lymphoma, bone marrow aspiration and chromosome analysis can also help establish the diagnosis.
Staging and grading
Most patients with follicular lymphoma present at an advanced stage, and most patients have bone marrow involvement at diagnosis. Staging is as follows:
Stage I – One involved lymph node or lymph node area
Stage II – Two or more involved lymph nodes or lymph node areas on the same side of diaphragm
Stage III – Involved lymph node or lymph node areas on both sides of diaphragm
Stage IV – Disseminated disease, such as bone marrow, liver, or central nervous system involvement
Follicular lymphoma is further categorized into grades according to the number of centroblasts per high-power field (hpf), as follows:
Grade 1 – 0-5 centroblasts per hpf
Grade 2 – 6-15 centroblasts per hpf
Grade 3 – > 15 centroblasts per hpf
Grade 3 disease is subdivided into grade 3A, in which centrocytes are present,
and grade 3B, in which folllicles composed of centrocytes are present. Clinically, grade 3B follicular lymphoma is treated like diffuse large B-cell lymphoma.
Management
Treatment varies based on the stage of the disease. Early-stage, localized disease may be treated with radiation therapy or excision in certain cases. Observation is recommended for patients with advanced disease until they develop systemic symptoms or disease that threatens organ function.
Multiagent chemotherapy in combination with rituximab is the most common first-line treatment strategy for follicular lymphoma. Combination chemotherapy regimens vary and include the following:
Rituximab, cyclophosphamide, vincristine, prednisone (R-CVP)
Rituximab, cyclophosphamide, doxorubicin, vincristine, prednisone (R-CHOP)
CHOP immediately followed by tositumomab/iodine-131 radioimmunotherapy (CHOP-RIT)
Bendamustine plus rituximab
Rituximab plus lenalidomide
(non-chemotherapeutic regimen)
Single agents tend to be less effective than combination chemotherapy, but are appropriate for selected patients because they may be simpler to administer, induce less toxicity, and palliate symptoms. Single agents include the following:
Chlorambucil
Fludarabine
Bendamustine
Rituximab
Tazemetostat
Idelalisib
Copanlisib
Duvelisib