Practice Essentials
Pancreatitis, an uncommon condition in pediatric patients, is characterized by inflammation of the pancreas, clinical signs of epigastric abdominal pain, and elevated serum digestive enzymes. The disease is associated with significant morbidity and mortality.
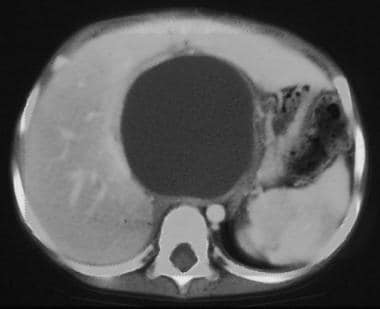
Pancreatitis can be local or diffuse and is classified as acute, chronic, inherited, necrotic, or hemorrhagic. Occasionally, pancreatitis is complicated by the formation of a fibrous-walled cavity filled with pancreatic enzymes, termed a pseudocyst (see the image below).
This computed tomography (CT) scan of the abdomen in the region of the pancreas demonstrates a large well-marginated cystic structure that represents a pancreatic pseudocyst.
Signs and symptoms
Most commonly, a child with acute pancreatitis presents with the following:
Abdominal pain (87%)
Vomiting (64%)
Abdominal tenderness (77%)
Abdominal distention (18%)
Less common clinical signs include the following:
Fever
Tachycardia
Hypotension
Jaundice
Abdominal guarding
Rebound tenderness
Decreased bowel sounds
Acute hemorrhagic pancreatitis
Physical examination findings associated with hemorrhagic pancreatitis may include a bluish discoloration of the flanks (ie, Grey Turner sign) or periumbilical region (ie, Cullen sign) because of blood accumulation in the fascial planes of the abdomen. Additional signs include pleural effusions, hematemesis, melena, and coma.
Chronic pancreatitis
Patients with chronic pancreatitis have recurrent episodes of upper abdominal pain associated with varying degrees of pancreatic dysfunction.
Pancreatic pseudocysts
Children with pancreatic pseudocysts may present with localized abdominal pain and a palpable, tender epigastric mass or abdominal fullness. Additional symptoms include the following:
Jaundice
Chest pain
Nausea
Vomiting
Anorexia
Weight loss
Fever
Ascites
Gastrointestinal (GI) hemorrhage (rarely)
See Clinical Presentation for more detail.
Diagnosis
Laboratory studies
Elevated amylase levels
Elevated lipase levels
Coagulopathy
Leukocytosis
Hyperglycemia
Glucosuria
Hypocalcemia
Hyperbilirubinemia
Elevated gamma glutamyl transpeptidase
Imaging studies
Ultrasonography: Primary screening tool for evaluation of the pediatric pancreas, due to the absence of ionizing radiation and the ability to image without sedation
Computed tomography (CT) scanning
Endoscopic retrograde cholangiopancreatography (ERCP)
Magnetic resonance cholangiopancreatography (MRCP)
Radiography
Histologic features
Acute pancreatitis: Focal areas of fat necrosis are interspersed with areas of interstitial hemorrhage secondary to the destruction of blood vessels
Chronic pancreatitis: Features include Intraglandular fibrosis, acinar cell destruction, lymphocytic infiltration, and pancreatic duct obstruction
Pancreatic pseudocysts: Localized collections of pancreatic secretions walled off by granulation tissue and lacking a true epithelial lining
See Workup for more detail.
Management
Acute pancreatitis should resolve in 2-7 days with adequate resuscitation, with management being predominantly supportive through the use of intravenous hydration, pain control, and bowel rest. Parenteral nutrition may be required for prolonged episodes.
In cases of intractable vomiting or ileus, nasogastric suction is indicated to aid intestinal-pancreatic rest by eliminating gastric secretions in the duodenum, the most potent activator of pancreatic secretion.
Because most resolve spontaneously, acute pancreatic pseudocysts smaller than 5 cm in diameter are managed with observation for 4-6 weeks. (Pancreatic pseudocysts larger than 5 cm in diameter may require surgical intervention.)
Surgery
Most surgical interventions are used in patients with chronic or relapsing pancreatitis. However, operative management of chronic pancreatitis in children is controversial. Indications for operative intervention include unsuccessful conservative medical therapy, intractable pain, impaired nutrition, and narcotic addiction. Surgical options include the following:
Distal pancreatectomy with Roux-en-Y pancreaticojejunostomy (ie, Duval procedure)
Lateral pancreaticojejunostomy (ie, Puestow procedure)
ERCP sphincteroplasty
Chronic pancreatic pseudocysts (>3 mo) are best treated surgically. Surgical approaches for internal drainage, as follow, are largely determined by the anatomic location of the pseudocyst:
Cystogastrostomy: If the pseudocyst is adherent to the posterior wall of the stomach
Cystoduodenostomy: If the cyst is present in the head of the pancreas
Cystojejunostomy: For cysts that are not adherent to the stomach or duodenum
Distal pancreatectomy: Considered when the pseudocyst is in the tail of the gland
Some authors suggest that endoscopic treatment should be the first interventional choice for pancreatic pseudocysts; the success rate for such therapy is as high as 85%. Other surgical procedures can be reserved for cases that fail endoscopic treatment.
See Treatment and Medication for more detail.