Practice Essentials
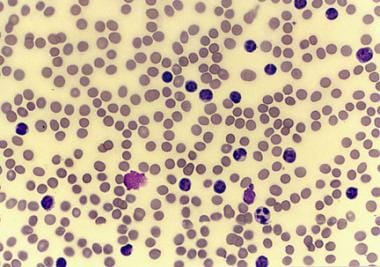
Chronic lymphocytic leukemia (chronic lymphoid leukemia, CLL) is a monoclonal disorder characterized by a progressive accumulation of functionally incompetent lymphocytes (see the histologic sample in the image below). CLL is the most common form of leukemia found in adults in Western countries.
Some patients die rapidly, within 2-3 years of diagnosis, because of complications from CLL, but most patients survive for 5-10 years.
Peripheral smear from a patient with chronic lymphocytic leukemia, small lymphocytic variety.
See Chronic Leukemias: 4 Cancers to Differentiate, a Critical Images slideshow, to help detect chronic leukemias and determine the specific type present.
Signs and symptoms
Patients with CLL present with a wide range of symptoms and signs. Onset is insidious, and it is not unusual for CLL to be discovered incidentally after a blood cell count is performed for another reason; 25-50% of patients will be asymptomatic at time of presentation.
Signs and symptoms include the following:
Enlarged lymph nodes, liver, or spleen
Recurring infections
Loss of appetite or early satiety
Abnormal bruising (late-stage sign)
Fatigue
Night sweats
See Presentation for more detail.
Diagnosis
Patients with CLL have a higher-than-normal white blood cell count, which is determined by complete blood count (CBC). Peripheral blood flow cytometry is the most valuable test to confirm a diagnosis of CLL. Other tests that may be helpful for diagnosis include bone marrow biopsy and ultrasonography of the liver and spleen. Immunoglobulin testing may be indicated for patients developing repeated infections.
Staging
Two staging systems are used for CLL.
The Rai-Sawitsky staging system categorizes patients into low-, intermediate-, and high-risk groups, as follows:
Low risk (formerly stage 0) – Lymphocytosis in the blood and marrow only (25% of presenting population)
Intermediate risk (formerly stages I and II) – Lymphocytosis with enlarged nodes in any site or splenomegaly or hepatomegaly (50% of presentation)
High risk (formerly stages III and IV) – Lymphocytosis with disease-related anemia (hemoglobin < 11 g/dL) or thrombocytopenia (platelets < 100 x 109/L) (25% of all patients)
The Binet staging system categorizes patients according to the number of lymph node groups involved, as follows:
Stage A – Hemoglobin 10 g/dL or higher, platelets 100 × 109/L or higher, and fewer than three lymph node areas involved.
Stage B – Hemoglobin and platelet levels as in stage A and three or more lymph node areas involved
Stage C – Hemoglobin less than 10 g/dL or platelets less than 100 × 109/L, or both
See Workup for more detail.
Management
Patients with early-stage CLL are not treated with chemotherapy until they become symptomatic or display evidence of rapid progression of disease. Early initiation of chemotherapy has failed to show benefit in CLL and may even increase mortality.
When chemotherapy is initiated, the nucleoside analogue fludarabine is the most commonly used first-line therapy in CLL. Combination regimens have shown improved response rates in several clinical trials and include the following:
Fludarabine, cyclophosphamide, and rituximab (FCR)
Pentostatin, cyclophosphamide, and rituximab (PCR)
Fludarabine, cyclophosphamide, and mitoxantrone (FCM)
Cyclophosphamide, vincristine, and prednisone (CVP)
Cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP)
Other agents used in treatment of CLL, most often for relapsed disease, include the following:
Duvelisib
Ibrutinib
Idelalisib
Obinutuzumab
Ofatumumab
Rituximab
Venetoclax
Allogeneic stem cell transplantation is the only known curative therapy for CLL.
See Treatment and Medication for more detail.
For patient education information, see Living With Chronic Lymphocytic Leukemia.