Overview
Introduction
Medical thoracoscopy or pleuroscopy is a minimally invasive endoscopic procedure utilized by pulmonologists to evaluate, diagnose, and treat plueral pathologies of the lung, mainly pleural effusions. The term thoracoscopy creates confusion because it refers to both the medical and surgical procedures. To avoid confusion, some authors suggest that medical thoracoscopy should be referred to as pleuroscopy. Thoracoscopy may be used exclusively for the surgical video-assisted thoracoscopic procedure (VATS).
Background
Medical thoracoscopy was initially performed in 1910 by an internist from Sweden named Hans-Christian Jacobaeus. Jacobaeus was the first to use the term thoracoscopy, which he described as “replacing fluid with air” in order to examine the pleural surfaces of two patients with tuberculous pleurisy. Jacobaeus later developed a therapeutic application for thoracoscopy by using thermocautery to lyse adhesions and create a pneumothorax to treat tuberculosis.
During the 1950s and 1960s, thoracoscopy gained popularity with pulmonologists because of the tuberculosis endemic in the United States. The major indications were for pleural and pulmonary biopsies for diffuse lung disease. However, with the advent of effective chemotherapy for tuberculosis, the need for thoracoscopy decreased. Surgeons adopted the procedure after advances in optics, laparoscopic techniques, and video technology. Thoracoscopy grew into the video-assisted thoracoscopic surgery that is currently performed by thoracic surgeons.
Indications
The accepted indications for medical thoracoscopy include the following:
Evaluation and diagnosis of idiopathic pleural effusions
Pleurodesis
Site-directed biopsy of parietal pleura
Staging of lung cancer
Staging for mesothelioma
Pleural effusion of unknown origin
Idiopathic pleural effusions that have been sampled by thoracentesis are ideal for medical thoracoscopy. The direct visualization of the pleura allows for site-directed biopsy of abnormal parietal pleura. Additionally, it allows for examination of the visceral pleura and any clues that may lead to the diagnosis of the pleural effusion. Most interventional pulmonologists limit biopsy to the parietal pleura due to the risk for injury to the lung when sampling the visceral pleura.
Cytologic examination of pleural fluid is diagnostic in only 60-80% of patients with metastatic pleural involvement and in less than 20% in patients with mesothelioma.
In cases for which the initial evaluation of a pleural effusion is nondiagnostic and malignancy is suspected, medical thoracoscopy and parietal pleural biopsy should be considered.
Medical thoracoscopy with pleural biopsy establishes a diagnosis in more than 90% of the cases.
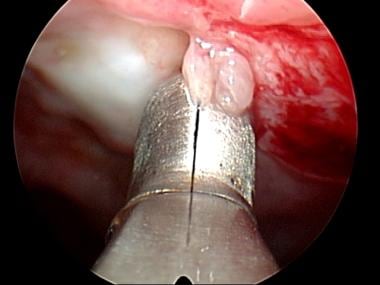
Biopsy forceps sampling parietal pleura.
Malignant pleural effusion/pleurodesis
In cases with an established malignant diagnosis, medical thoracoscopy also has a therapeutic role in the form of pleurodesis.
Complete evacuation of pleural fluid, with maximization of lung expandability by removing adhesions and pleurodesis by talc insufflations has short- and long-term success rates greater than 90%.
Talc pleurodesis on lung and parietal pleura.
The benefits of pleurodesis include improvement of functional status as well as improving the quality of life, especially for patients with advanced malignant disease. In patients who are undergoing further treatment for malignancy, improving the functional status may allow for increased treatment options overall.
In addition, patients who do require further treatment can be excluded from certain chemotherapeutics because of chemotherapeutic tendency to distribute into the pleural effusion and affect serum levels. The classic examples of this are methotrexate, fludarabine, and possibly pemetrexed.
Survival of patients with advanced pleural disease is often limited, from weeks to months. The benefits of medical thoracoscopy versus repeated thoracentesis should be carefully considered for the individual patient.
Lung cancer
In the patient with known lung cancer and an effusion with a negative cytology, medical thoracoscopy is an excellent tool. It allows for direct visualization of the pleura and a thorough examination for evidence of metastasis.
Bulky metastasis on parietal pleura.
Examination for evidence of metastasis.
The sensitivity of pleuroscopy-guided biopsy in malignant pleural effusions is 95%, compared with 62% for cytology from thoracentesis and 44% for closed pleural biopsy.
By allowing for a more accurate diagnosis and staging, unnecessary procedures may be prevented on a patient who is inappropriately categorized into a lower stage.
Malignant mesothelioma
The yield of cytology for malignant mesothelioma is even lower than most malignant effusions, as low as 41% in one study.
It can be difficult to reach a definitive diagnosis without complete visualization of the pleural space. Medical thoracoscopy is favored over thoracotomy for two reasons. First, the pleural specimen obtained with the minimally invasive 5-mm forceps is comparable to the specimen achieved with open biopsies. Second, the site-directed nature of pleural biopsies through the semirigid pleuroscope allows for a minimally invasive approach.
Tuberculous pleural effusion
There is controversy regarding if medical thoracoscopy is warranted when the suspicion for tuberculosis is high. In these cases, the diagnostic yield from closed-needle pleural biopsy is approximately 69%, with some studies reporting rates as high as 88%.
The consensus is that medical thoracoscopy should be reserved for special circumstances, such as lysis of adhesions or more effective drainage of loculated effusions, as well as when larger quantities of tissue are needed for sensitivities.
Recurrent pleural effusions of benign origin
Recurrent pleural effusions are often caused by heart failure, cardiac surgery, nephritic syndrome, connective tissue diseases, and other inflammatory disorders. When these effusions are not well controlled by repeat large-volume thoracentesis, pleural biopsies can be obtained through medical thoracoscopy, and pleurodesis can be performed if necessary.
Empyema and complicated parapneumonic effusions
Some interventional pulmonologists have used medical thoracoscopy for drainage of uncomplicated empyema and chest tube placement. Additionally, it can be used carefully for lysis of thin fibrous adhesions.
Pleural adhesions on medical thoracoscopy.
Currently, this is not routinely performed or the standard of care, mainly because timing is key in these procedures and they should be considered early if chest tube drainage is inadequate.
In later stages of the empyema, there may be thick fibrous adhesions, pleural peel, or trapped lung. In these cases, video-assisted thoracoscopic decortication is required for treatment.
Pneumothorax
Medical thoracoscopy can offer definitive treatment or diagnostic inspection of a patient with a recurrent pneumothorax. In patients who are not candidates for video-assisted thoracoscopic surgery, pleural abrasion or talc pleurodesis can be performed. For patients suitable for video-assisted thoracoscopic surgery, bullectomy, pleural abrasion, and pleurectomy in the operating room are superior and preferred.
Contraindications
The major contraindications are related to the ability to perform the procedure. As long as no contraindication exists for the ability to insert instruments into the pleural space, it can be performed safely. Even when the lung is adherent to the chest wall, the use of transthoracic ultrasound by interventional pulmonologists can allow identification of safe areas to insert the trocar and pleuroscope.
A pleural separation of at least 10 mm is recommended to minimize injury to the lung. In patients with small effusions, a pneumothorax may need to be induced by cannulating the pleural space and asking the patient to inspire deeply while the catheter is open to the atmosphere. The presence of a pneumothorax can then be confirmed with either chest radiograph or thoracic ultrasound at the bedside. This procedure is limited by the ability of the patient to tolerate a pneumothorax. In patients who already have an effusion, the concern regarding tolerance of a pneumothorax is not as worrisome because an equal volume of fluid would be replaced by air.
The following relative contraindications may be corrected and accounted for:
Refractory cough
Hypoxia
Coagulopathy
Thrombocytopenia