Practice Essentials
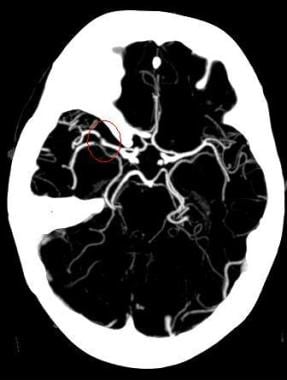
Ischemic stroke (see the image below) is characterized by the sudden loss of blood circulation to an area of the brain, resulting in a corresponding loss of neurologic function. Acute ischemic stroke is caused by thrombotic or embolic occlusion of a cerebral artery and is more common than hemorrhagic stroke.
Maximum intensity projection (MIP) image from a computed tomography angiogram (CTA) demonstrates a filling defect or high-grade stenosis at the branching point of the right middle cerebral artery (MCA) trunk (red circle), suspicious for thrombus or embolus. CTA is highly accurate in detecting large- vessel stenosis and occlusions, which account for approximately one third of ischemic strokes.
See Acute Stroke, a Critical Images slideshow, for more information on incidence, presentation, intervention, and additional resources.
Signs and symptoms
Consider stroke in any patient presenting with acute neurologic deficit or any alteration in level of consciousness. Common stroke signs and symptoms include the following:
Abrupt onset of hemiparesis, monoparesis, or (rarely) quadriparesis
Hemisensory deficits
Monocular or binocular visual loss
Visual field deficits
Diplopia
Dysarthria
Facial droop
Ataxia
Vertigo (rarely in isolation)
Nystagmus
Aphasia
Sudden decrease in level of consciousness
Although such symptoms can occur alone, they are more likely to occur in combination. No historical feature distinguishes ischemic from hemorrhagic stroke, although nausea, vomiting, headache, and sudden change in level of consciousness are more common in hemorrhagic strokes. In younger patients, a history of recent trauma, coagulopathies, illicit drug use (especially cocaine), migraines, or use of oral contraceptives should be elicited.
With the availability of reperfusion options (fibrinolytic and endovascular therapies) for acute ischemic stroke in selected patients, the physician must be able to perform a brief but accurate neurologic examination on patients with suspected stroke syndromes. The goals of the neurologic examination include the following:
Confirming the presence of stroke symptoms (neurologic deficits)
Distinguishing stroke from stroke mimics
Establishing a neurologic baseline, should the patient’s condition improve or deteriorate
Establishing stroke severity, using a structured neurologic exam and score (National Institutes of Health Stroke Scale [NIHSS]) to assist in prognosis and therapeutic selection
Essential components of the neurologic examination include the following evaluations:
Cranial nerves
Motor function
Sensory function
Cerebellar function
Gait
Deep tendon reflexes
Language (expressive and receptive capabilities)
Mental status and level of consciousness
The skull and spine also should be examined, and signs of meningismus should be sought.
See Clinical Presentation for more detail.
Diagnosis
Emergent brain imaging is essential for evaluation of acute ischemic stroke. Noncontrast computed tomography (CT) scanning is the most commonly used form of neuroimaging in the acute evaluation of patients with apparent acute stroke. The following neuroimaging techniques may also be used emergently:
CT angiography and CT perfusion scanning
Magnetic resonance imaging (MRI)
Carotid duplex scanning
Digital subtraction angiography
Lumbar puncture
A lumbar puncture is required to rule out meningitis or subarachnoid hemorrhage when the CT scan is negative but the clinical suspicion remains high
Laboratory studies
Laboratory tests performed in the diagnosis and evaluation of ischemic stroke include the following:
Complete blood count (CBC): A baseline study that may reveal a cause for the stroke (eg, polycythemia, thrombocytosis, leukemia), provide evidence of concurrent illness, and ensure absence of thrombocytopenia when considering fibrinolytic therapy
Basic chemistry panel: A baseline study that may reveal a stroke mimic (eg, hypoglycemia, hyponatremia) or provide evidence of concurrent illness (eg, diabetes, renal insufficiency)
Coagulation studies: May reveal a coagulopathy and are useful when fibrinolytics or anticoagulants are to be used
Cardiac biomarkers: Important because of the association of cerebral vascular disease and coronary artery disease
Toxicology screening: May assist in identifying intoxicated patients with symptoms/behavior mimicking stroke syndromes or the use of sympathomimetics, which can cause hemorrhagic and ischemic strokes
Pregnancy testing: A urine pregnancy test should be obtained for all women of childbearing age with stroke symptoms; recombinant tissue-type plasminogen activator (rt-PA) is a pregnancy class C agent
See Workup for more detail.
Management
The goal for the emergent management of stroke is to complete the following within 60 minutes or less of patient arrival:
Assess airway, breathing, and circulation (ABCs) and stabilize the patient as necessary
Complete the initial evaluation and assessment, including imaging and laboratory studies
Initiate reperfusion therapy, if appropriate
Critical treatment decisions focus on the following:
The need for airway management
Optimal blood pressure control
Identifying potential reperfusion therapies (eg, intravenous fibrinolysis with rt-PA (alteplase) or intra-arterial approaches)
Involvement of a physician with a special interest and training in stroke is ideal. Stroke care units with specially trained nursing and allied healthcare personnel have clearly been shown to improve outcomes.
Ischemic stroke therapies include the following:
Fibrinolytic therapy
Antiplatelet agents
Mechanical thrombectomy
Treatment of comorbid conditions may include the following:
Reduce fever
Correct hypotension/significant hypertension
Correct hypoxia
Correct hypoglycemia
Manage cardiac arrhythmias
Manage myocardial ischemia
Stroke prevention
Primary stroke prevention refers to the treatment of individuals with no previous history of stroke. Measures may include use of the following:
Platelet antiaggregants
Statins
Exercise
Lifestyle interventions (eg, smoking cessation, alcohol moderation)
Secondary prevention refers to the treatment of individuals who have already had a stroke. Measures may include use of the following:
Platelet antiaggregants
Antihypertensives
Statins
Lifestyle interventions
See Treatment and Medication for more detail.