Overview
The primary purpose of impedance audiometry is to determine the status of the tympanic membrane and middle ear via tympanometry. The secondary purpose of this test is to evaluate acoustic reflex pathways, which include cranial nerves (CN) VII and VIII and the auditory brainstem. This test cannot be used to directly assess auditory sensitivity, although results are interpreted in conjunction with other threshold measures.
Acoustic immittance is a measurement of energy or air pressure flow, which involves the ear canal, eardrum, ossicular chain, tensor tympani, stapedius muscle, cochlea, CNs VII and VIII, and the brainstem. Mass, mobility, and resistance of the outer and middle ear systems affect this test. The reciprocal of acoustic immittance is acoustic impedance. Particularly in earlier years, these measurements were performed in impedance rather than immittance measures; thus, the term impedance audiometry is sometimes used.
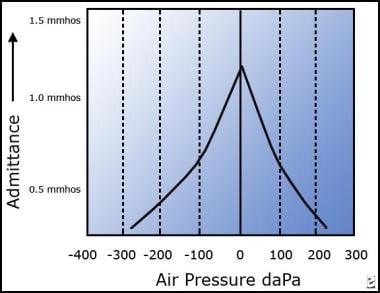
The image below depicts a type A tympanogram, suggesting normal function.
Type A tympanogram suggesting normal function.
Acoustic immittance tests
The following tests are included in the category acoustic immittance tests:
Tympanometry (most commonly used)
Perilymphatic fistula test (efficacy questionable)
Acoustic reflex thresholds
Acoustic reflex decay
Acoustic reflex thresholds
An acoustic reflex threshold is a middle ear measurement of stapedius muscle response to higher intensity and adequate duration sounds for individual frequencies. Consider the softest sound that elicits a reflex contraction of the stapedius muscle as the acoustic reflex threshold. When the stapedius muscle contracts in response to a loud sound, that contraction changes the middle ear immittance. This change in immittance can be detected as a deflection in the recording.
Tympanometry records changes in middle ear immittance, while air pressure is varied in the ear canal and acoustic reflexes are recorded at a single air pressure setting (ie, the pressure setting that provided the peak immittance reading for that particular ear on the tympanogram). Ear canal pressure is maintained at that specific setting, while tones of various intensities are presented into the ear canal and immittance is recorded. A significant change in middle ear immittance immediately after the stimulus is considered an acoustic reflex.
A stapedial muscle contraction in response to an intense signal occurs bilaterally in normal ears with either unilateral or bilateral stimulation. This reaction occurs because the stapedial reflex pathway has both ipsilateral and contralateral projections. Acoustic reflex thresholds generally are determined in response to stimuli of 500, 1000, 2000, and 4000 Hz. For screening purposes, or for a general check of the pathway’s integrity, usually test at 1000 Hz.
Types of acoustic reflex
For the ipsilateral or uncrossed acoustic reflex, stimulate the ear that is monitored for response. The assessed pathway involves the cochlea, ventral cochlear nucleus, CN VIII, CN VII and its motor nucleus, and the stapedius muscle—all on the side ipsilateral to the stimulus.
For the contralateral or crossed acoustic reflex, present the stimulus to the ear opposite the ear that is monitored for response. The assessed pathway involves the ipsilateral cochlea, ventral cochlear nucleus, and CN VIII; the pathway crosses the trapezoid body and then involves the contralateral medial superior olive, CN VII and its motor nucleus, and the stapedius muscle.
Variability of acoustic reflex thresholds
Thresholds vary according to individual hearing sensitivity and retrocochlear function. The range for acoustic reflexes in individuals with normal hearing averages 70-100 decibel (dB) sound pressure level (SPL). The greater the hearing loss, the higher the acoustic reflex threshold for conductive hearing loss. For sensorineural hearing loss, acoustic reflex thresholds may be within the normal range, particularly for mild-to-moderate hearing losses with recruitment.
Elevated or absent acoustic reflex thresholds (ie, >100 dB SPL) for any given frequency may suggest sensorineural or conductive hearing loss, facial nerve disorder, or middle ear disorder. Reflexes usually are absent or cannot be recorded if the patient has type B tympanograms; therefore, acoustic reflexes generally are not tested in these ears.
For example, if the ear canal is occluded with cerumen, a type B tympanogram with low volume will be recorded. In this case, acoustic reflexes cannot be measured because middle ear immittance is not being measured. (Cerumen blocks the signal.)
For a type B tympanogram with normal volume (as in otitis media) no pressure peak for immittance is obtained. The pressure between the ear canal and middle ear are not equilibrated, and acoustic reflexes cannot be recorded.
For a type B tympanogram with high volume (as in the presence of patent pressure equalization tubes or perforated tympanic membranes), an open exchange of air occurs between the ear canal and middle ear; thus, any contraction of the stapedius muscle cannot be measured.
Relevant Anatomy
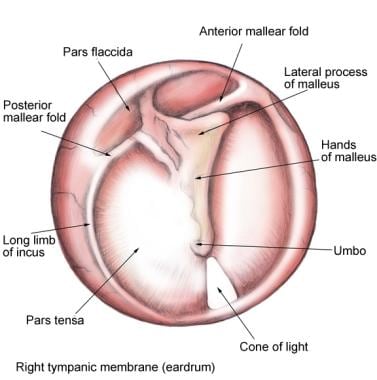
The tympanic membrane is an oval, thin, semi-transparent membrane that separates the external and middle ear (tympanic cavity). The tympanic membrane is divided into 2 parts: the pars flaccida and the pars tensa. The manubrium of the malleus is firmly attached to the medial tympanic membrane; where the manubrium draws the tympanic membrane medially, a concavity is formed. The apex of this concavity is called the umbo. The area of the tympanic membrane superior to the umbo is termed the pars flaccida; the remainder of the tympanic membrane is the pars tensa (see the image below).
Tympanic membrane (TM): pars flaccida (superior to insertion manubrium) and pars tensa (remainder of TM).
The eighth cranial nerve (CN VIII) or vestibulocochlear nerve is composed of 2 different sets of fibers: (1) the cochlear nerve and (2) the vestibular nerve. These 2 nerves are anatomically and physiologically different. The peripheral segments of the cochlear and vestibular nerves join at the lateral part of the internal auditory canal (IAC) to form the vestibulocochlear nerve. They are also joined by the facial nerve in the IAC. The length of the vestibulocochlear nerve, from the glial-Schwann junction to the brainstem, is 10-13 mm in the human male and 7-10 mm in females.
For more information about the relevant anatomy, see Ear Anatomy and Auditory System Anatomy.