Practice Essentials
Hypoglycemia is characterized by a reduction in plasma glucose concentration to a level that may induce symptoms or signs such as altered mental status and/or sympathetic nervous system stimulation. This condition typically arises from abnormalities in the mechanisms involved in glucose homeostasis. The most common cause of hypoglycemia in patients with diabetes is injecting a shot of insulin and skipping a meal or overdosing insulin.
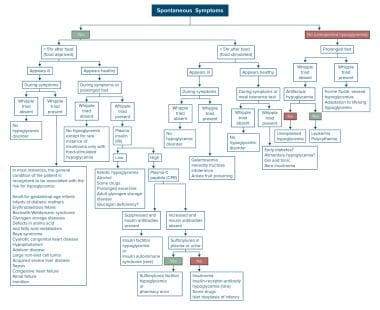
The image below depicts a diagnostic algorithm for hypoglycemia.
Diagnostic algorithm. A systematic approach is often required to establish the true cause of hypoglycemia, using an algorithmic approach.
Signs and symptoms of hypoglycemia
The glucose level at which an individual becomes symptomatic is highly variable (threshold generally at < 50 mg/dL). Carefully review the patient’s medication and drug history for potential causes of hypoglycemia (eg, new medications, insulin usage or ingestion of an oral hypoglycemic agent, possible toxic ingestion).
The patient’s medical and/or social history may reveal the following:
Diabetes mellitus, renal insufficiency/failure, alcoholism, hepatic cirrhosis/failure, other endocrine diseases, or recent surgery
Central nervous system: Headache, confusion, personality changes
Ethanol intake and nutritional deficiency
Weight reduction, nausea and vomiting
Fatigue, somnolence
Neurogenic or neuroglycopenic symptoms of hypoglycemia may be categorized as follows:
Neurogenic (adrenergic) (sympathoadrenal activation) symptoms: Sweating, shakiness, tachycardia, anxiety, and a sensation of hunger
Neuroglycopenic symptoms: Weakness, tiredness, or dizziness; inappropriate behavior (sometimes mistaken for inebriation), difficulty with concentration; confusion; blurred vision; and, in extreme cases, coma and death
Reactive hypoglycemia includes the following features:
More common in overweight and obese people who are insulin-resistant
May be a frequent precursor to type 2 diabetes
Possible higher risk in patients with a family history of type 2 diabetes or insulin-resistance syndrome
True loss of consciousness is highly suggestive of an etiology other than reactive hypoglycemia.
Gestational hypoglycemia may have the following features
:
More frequent in women younger than 25 years
More frequent in women with a preexisting medical condition
Less frequent in women whose prepregnancy body mass index was ≥30 kg/m2
Greater risk of preeclampsia/eclampsia in affected women
See Clinical Presentation for more detail.
Diagnosis of hypoglycemia
Rapid diagnosis and treatment is essential in any patient with suspected hypoglycemia, regardless of the cause. The Whipple triad is characteristically present: documentation of low blood sugar, presence of symptoms, and reversal of these symptoms when the blood glucose level is restored to normal.
Physical findings, however, are nonspecific in hypoglycemia and are generally related to the central and autonomic nervous systems. Examination includes the following:
Vital signs
Head, eyes, ears, nose, and throat
Cardiovascular
Neurologic
Pulmonary
Gastrointestinal
Dermatologic
Elderly persons exhibit fewer symptoms of hypoglycemia, and their threshold of plasma glucose is lower at presentation than in younger persons.
Laboratory studies
Patients with no previous history of hypoglycemia require a complete workup to find a potentially treatable disease. Laboratory studies that should be obtained include the following:
Glucose and electrolyte levels (including calcium, magnesium)
Oral glucose tolerance test and/or 72-hour fasting plasma glucose
Complete blood count
Other tests that may be helpful including the following:
Blood cultures
Urinalysis
Serum insulin, cortisol levels, and thyroid hormone levels
C-peptide levels
Proinsulin
Imaging studies
Imaging modalities to evaluate insulinomas may include the following:
CT scanning
MRI
Octreotide scanning
Procedures
Selective percutaneous transhepatic venous sampling may be performed to localize an insulinoma to the pancreatic head, body, or tail. Selective arteriography is also often helpful in localizing insulin-secreting lesions.
See Workup for more detail.
Management of hypoglycemia
Pharmacotherapy
The mainstay of therapy for hypoglycemia is glucose. Other medications may be administered based on the underlying cause or the accompanying symptoms.
Medications used in the treatment of hypoglycemia include the following:
Glucose supplements (eg, dextrose)
Glucose-elevating agents (eg, glucagon, glucagon intranasal)
Inhibitors of insulin secretion (eg, diazoxide, octreotide)
Antineoplastic agents (eg, streptozocin)
Other therapies
Fasting hypoglycemia: Dietary therapy (frequent meals/snacks preferred, especially at night, with complex carbohydrates); IV glucose infusion; IV octreotide
Reactive hypoglycemia: Dietary therapy (restriction of refined carbohydrates, avoidance of simple sugars, increased meal frequency, increased protein and fiber); alpha-glucosidase inhibitors
Surgery
Definitive treatment for fasting hypoglycemia caused by a tumor is surgical resection. The success rate is good for benign islet-cell adenomas, and the success rate for malignant islet-cell tumors can be as high as 50%.
See Treatment and Medication for more detail.