Practice Essentials
Although hirsutism is broadly defined as excessive hairiness, the common clinical use of the term refers to women with excess growth of terminal hair in a male pattern. In this sense, hirsutism is one of the most common endocrine disorders, affecting approximately 10% of women in the United States. In these women, the hairiness implies the presence of abnormal androgen action, which may represent a serious or, more likely, a nonserious medical problem. Regardless of the etiology, hirsutism can produce mental trauma and emotional anguish.
Even mild cases of hirsutism may be viewed by the patient and others as a presumptive loss of femininity. In more severe cases, hirsutism can be a serious cosmetic problem. The major objectives in the management of hirsutism are to rule out a serious underlying medical condition and to devise a plan of treatment.
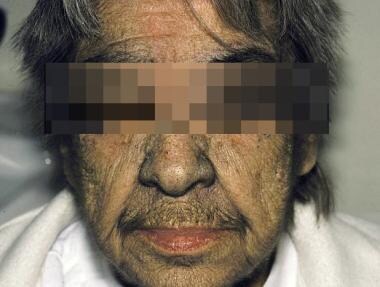
Idiopathic hirsutism in an elderly woman is shown in the photo below.
Idiopathic hirsutism in an elderly woman.
Workup in hirsutism
Approximately 50% of women with even minimal hirsutism have excessive androgen. Laboratory studies in hirsutism serve both to confirm the clinical impression of hyperandrogenism and to identify the source of excess androgens, either adrenal or ovarian.
The most important assay is the level of serum testosterone, the major circulating androgen. If the total serum testosterone level is normal, measure the free serum level because hyperandrogenism (and insulin resistance, if present) decreases sex steroid-binding globulin, such that the unbound, biologically active testosterone moiety may be elevated even if the total level is unremarkable.
If indicated based on the findings from the clinical evaluation and laboratory testing, perform ovarian ultrasonography and adrenal computed tomography (CT) scanning or magnetic resonance imaging (MRI) to evaluate for either ovarian or adrenal sources of androgen production.
Management of hirsutism
The treatment of hirsutism begins with a careful explanation about the cause of the problem and reassurance that the patient is not losing her femininity. Then, direct intervention, if possible, is instituted for the underlying disorder. If hirsutism persists (or the patient has idiopathic hirsutism), other cosmetic or systemic treatment may be necessary. In some cases, cosmetic measures may be sufficient. In others, the slow progress of systemic therapy may necessitate more immediate cosmetic treatment. The most effective strategy is to combine systemic therapy, which has a slow onset of effectiveness, with mechanical depilation (shaving, plucking, waxing, depilatory creams) or light-based (laser or pulsed-light) hair removal.
Systemic therapies directed at hirsutism can be divided into those that decrease ovarian or adrenal androgen production and those that inhibit androgen action in the skin. The systemic therapies include glucocorticoids, oral contraceptives (OCs), spironolactone, flutamide, finasteride, cyproterone acetate (not available in the United States), and insulin sensitizers (metformin and rosiglitazone).
Laser therapy has been shown not only to reduce unwanted hair but also to improve depression and anxiety in women with hirsutism. In many patients, hirsutism can be controlled just with laser, without using any drugs.